超声误诊无功能性甲状旁腺囊肿1例
2019-05-20 余芬 杨顺实 中国医学影像技术
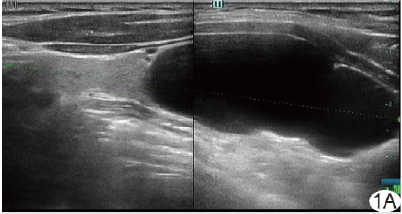
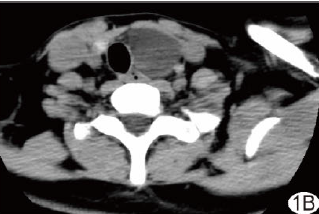
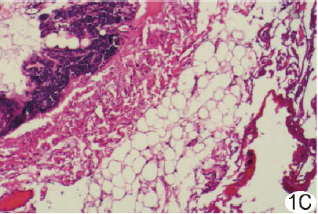
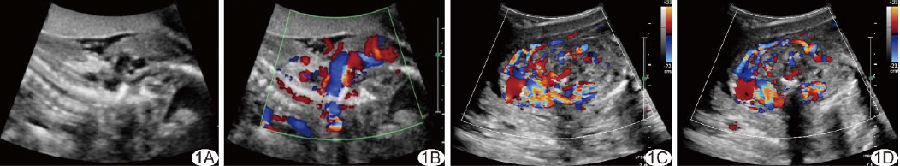
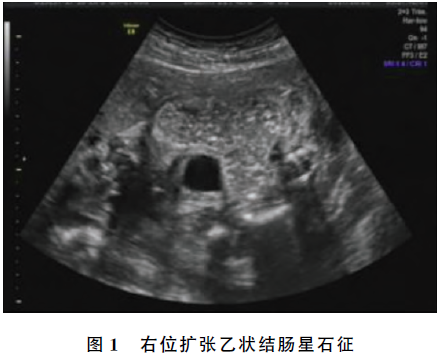
患者女,53岁,因“无意中发现左侧颈部鸡蛋大肿块1个月”就诊。患者无发热、颈部胀痛,无声嘶、呛咳,无怕热、多汗、手足麻木等症状。超声检查:甲状腺左侧叶下方可见一无回声区,大小约5.7 cm×2.1 cm×2.9 cm,下缘向下延伸至锁骨后方。超声诊断为甲状腺左侧叶下方囊性包块,疑来源于纵隔(图1A)。CT检查:甲状腺左侧叶下极见一囊状低密度影,延伸至上纵隔,边缘光滑清晰,大小约3.4 cm×2.6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#功能性#
39
#无功能性#
37
#甲状旁腺囊肿#
40
#囊肿#
33
#甲状旁腺#
41