Diabetologia:FAK酪氨酸磷酸化受AMPK调节并控制人骨骼肌的代谢
2018-04-24 MedSci MedSci原创
近日,国际杂志 《Diabetologia》上在线发表一项关于FAK酪氨酸磷酸化受AMPK调节并控制人骨骼肌的代谢的研究。 胰岛素介导的信号和AMP激活的蛋白激酶(AMPK)介导的信号分别在能量充足和不足的生理条件被激活。粘着斑激酶(FAK)涉及胰岛素信号传导和各种非肌肉细胞类型的癌症进展,并在骨骼肌分化过程中起调节作用。FAK在骨骼肌中与胰岛素刺激或AMPK活化有关的作用尚不清楚。研究人员
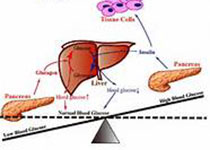
近日,国际杂志 《Diabetologia》上在线发表一项关于FAK酪氨酸磷酸化受AMPK调节并控制人骨骼肌的代谢的研究。 胰岛素介导的信号和AMP激活的蛋白激酶(AMPK)介导的信号分别在能量充足和不足的生理条件被激活。粘着斑激酶(FAK)涉及胰岛素信号传导和各种非肌肉细胞类型的癌症进展,并在骨骼肌分化过程中起调节作用。FAK在骨骼肌中与胰岛素刺激或AMPK活化有关的作用尚不清楚。研究人员检测了胰岛素或AMPK活化对人骨骼肌FAK磷酸化的影响以及FAK对葡萄糖和脂质代谢的直接作用。研究人员假设胰岛素治疗和AMPK激活会对FAK磷酸化产生相反的作用,并且沉默FAK基因会改变新陈代谢。研究人员用胰岛素或AMPK活化化合物5-氨基咪唑-4-甲酰胺核糖核苷酸(AICAR)处理人肌肉以确定FAK磷酸化和葡萄糖转运。使用原代人骨骼肌细胞研究胰岛素或AICAR处理对血清饥饿期间FAK信号传导的影响,以及确定FA K沉默基因PTK2的代谢结果。 研究发现,AMPK的活化降低了骨骼肌中FAK的酪氨酸磷酸化。在分离的人骨骼肌和培养的肌管中AICAR降低了p-FAK Y397。胰岛素刺激不会改变FAK磷酸
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#FAK#
37
#BET#
32
#DIA#
42
#骨骼肌#
34
学习了.谢谢分享!
43