Open Forum Infect Dis:门诊感染防控,你准备好了吗?(附评估表)
2018-06-19 梁丹燕 SIFIC感染官微
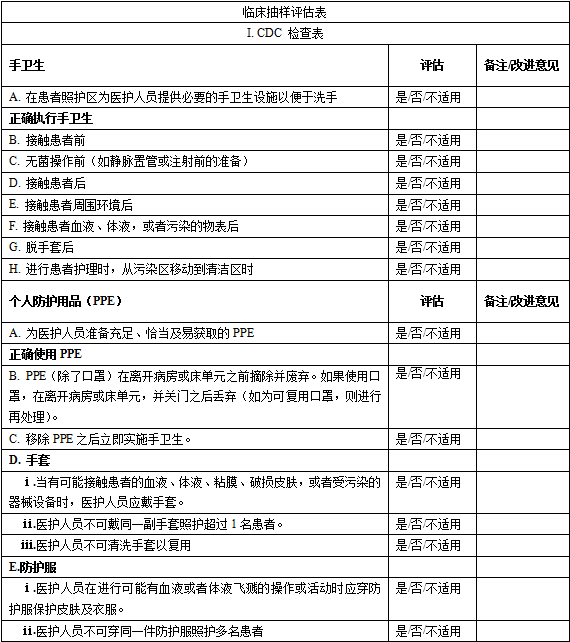
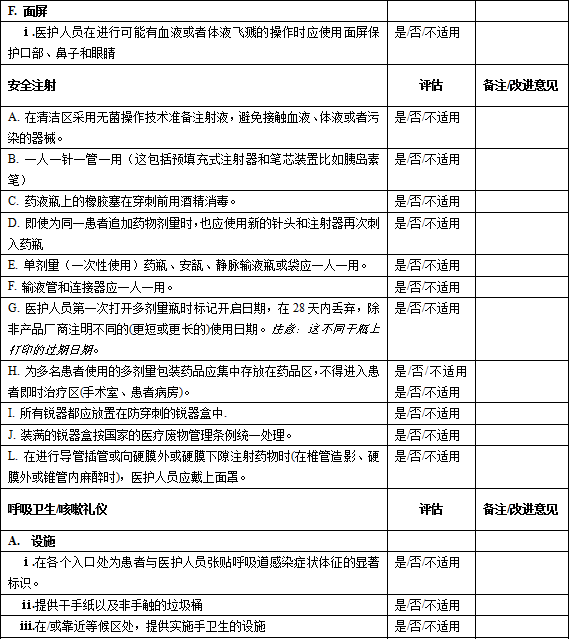
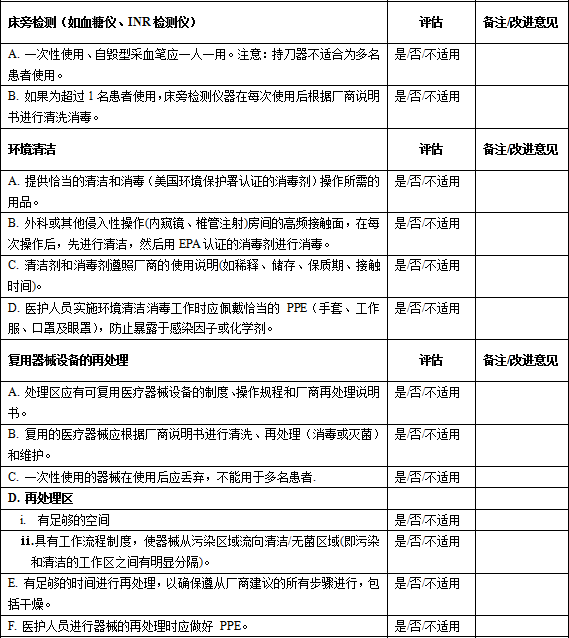
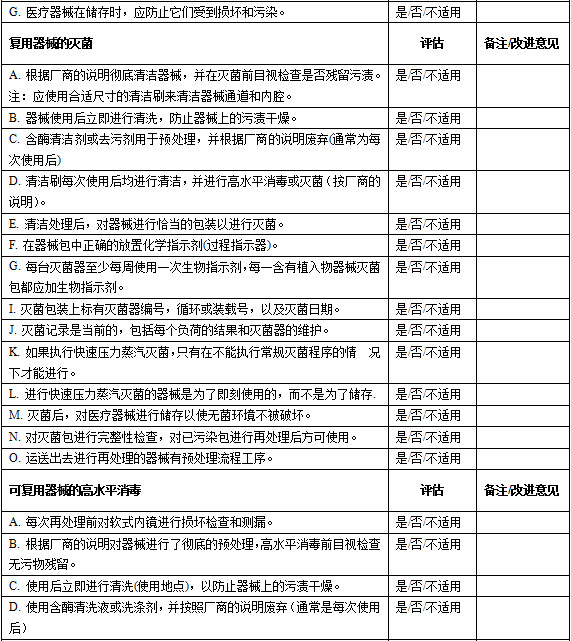
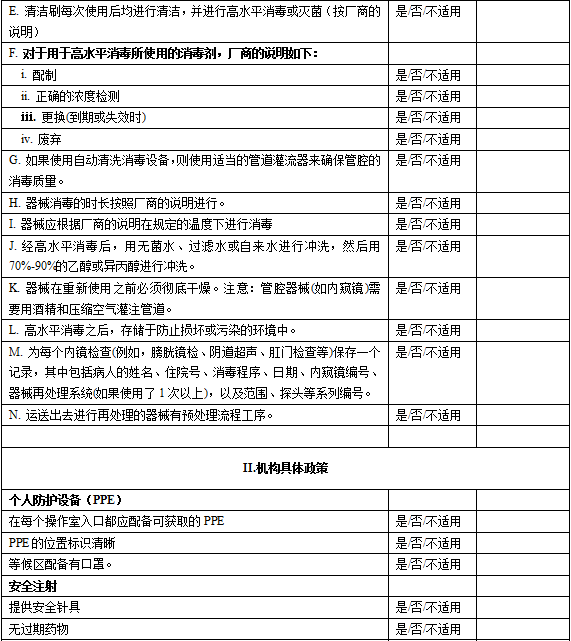
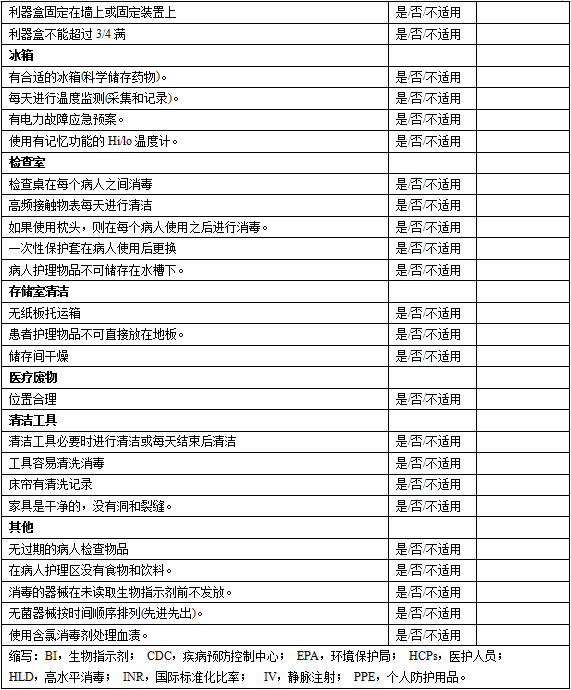
随着越来越多的患者诊疗工作在门诊开展,医疗保健相关感染和暴发的机会也随之增加。国际的相关机构也已经注意到这一感染暴发新地点,早期的指南,关注的多为传染病,如艾滋病、乙肝丙肝等。但即便有指南出台,门诊相关感染的暴发仍层出不穷,究其原因,多与不遵从指南有关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
41
#Dis#
47
#感染防控#
52
学习学习.了解了解
0
学习了
71
看看
53