Stroke:卒中后下肢运动障碍的比例恢复
2017-03-26 xing.T MedSci原创
由此可见,卒中后3个月下肢损伤恢复约70%。缺乏合适的群体可能是因为上肢和下肢的下行运动传导束存在解剖组织的差异。下肢比例恢复不会受到治疗剂量的影响,提供了进一步的证据表明它反映了一个基本的生物学过程。
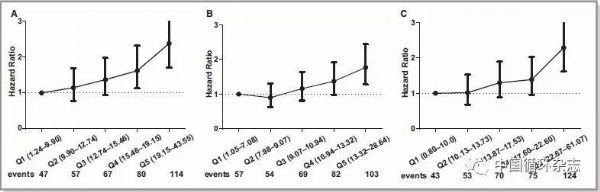
在卒中后皮质脊髓束(CST)功能正常的患者中,上肢功能损伤再3个月内恢复约为70%,这就是所谓的比例恢复规则。然而卒中后没有CST功能的患者则不符合这一规则,并且有更糟糕的上肢结局。近日,卒中领域权威杂志Stroke上发表了一篇荟萃文章,研究人员探究了下肢(LL)运动障碍的恢复情况。
研究人员采用下肢Fugl-Meyer运动功能量表评定了卒中患者3天和30天后的下肢无力情况。CST的完整性是在一个使用经颅磁刺激测试LL运动诱发电位和磁共振成像测量CST病变负荷的子集中确定。研究人员采用线性回归分析来预测运动功能障碍的恢复情况(ΔFugl-Meyer)包括初始损伤因素、运动诱发电位状态、CST损伤负荷以及下肢治疗剂量。
该研究有32例患者完成了3个月的随访,下肢初始运动损伤恢复了74%(95%可信区间为60%-88%)。初始损伤是唯一的运动损伤恢复显著预测因子。没有确定的患者群体不适合比例恢复规则。CST完整性的指标不能预测比例下肢恢复情况。
由此可见,卒中后3个月下肢损伤恢复约70%。缺乏合适的群体可能是因为上肢和下肢的下行运动传导束存在解剖组织的差异。下肢比例恢复不会受到治疗剂量的影响,提供了进一步的证据表明它反映了一个基本的生物学过程。
原始出处:
Marie-Claire Smith,et al. Proportional Recovery From Lower Limb Motor Impairment After Stroke.Stroke. 2017. https://doi.org/10.1161/STROKEAHA.116.016478
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#卒中后#
26
#运动障碍#
32
好好学习,涨知识
56
学习了
59
学习一下
61
学习了,值得分享
66
中国实际比例低于70%,可能与卒中严重,错失溶栓机会,后期康复不系统有关
53