Blood:Bcor剂量不足可促进骨髓增生异常综合征的发生发展
2018-09-21 MedSci MedSci原创
中心点:Bcor剂量不足会促进骨髓增生异常综合征的发生发展。在骨髓增生异常综合征的病理过程中,Bcor剂量不足与Tet2缺失相互协作。摘要:BCOR,编码BCL-6共抑制剂(BCOR),与X染色体连锁,是多种血液恶性肿瘤(包括骨髓增生异常综合征)的体细胞突变靶点。Shiro Tara等人既往发现造血室缺失Bcor4号外显子的小鼠(BcorΔE4/y)会进展出NOTCH依赖性的急性T细胞淋巴细胞白血
Bcor剂量不足会促进骨髓增生异常综合征的发生发展。
在骨髓增生异常综合征的病理过程中,Bcor剂量不足与Tet2缺失相互协作。
摘要:
BCOR,编码BCL-6共抑制剂(BCOR),与X染色体连锁,是多种血液恶性肿瘤(包括骨髓增生异常综合征)的体细胞突变靶点。Shiro Tara等人既往发现造血室缺失Bcor4号外显子的小鼠(BcorΔE4/y)会进展出NOTCH依赖性的急性T细胞淋巴细胞白血病(T-ALL)。
现Shiro Tara等人对缺乏Bcor9/10号外显子的小鼠(BcorΔE9-10/y)进行分析,BcorΔE9-10/y小鼠表达C端截短的BCOR,不能与多梳抑制复合物(PRC)1.1的核心效应元件相互作用。BcorΔE9-10/y小鼠表现为致死性T-ALL,与BcorΔE4/y小鼠类似,只不过BcorΔE9-10/y小鼠的粒细胞表现出生长优势,而且敲除Tet2时得到进一步加强。
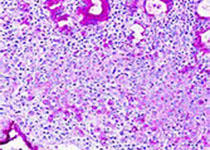
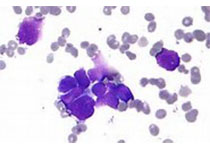
Tet2Δ/ΔBcorΔE9-10/y小鼠可发展成致死性MDS,伴随进行性贫血和白细胞减少、无效造血和血细胞形态异常。在次级接受者体内,Tet2Δ/ΔBcorΔE9-10/y MDS细胞可产生MDS,或进展成致死性MDS/MPN。
转录谱分析显示Cebpa家族和Hoxa集基因的髓系调控基因在BcorΔE9-10/y前体细胞中脱抑制,P53靶基因在MDS有核红细胞中特异性激活,导致大量细胞凋亡。
总而言之,本研究揭示了BCOR在髓系恶性肿瘤中的肿瘤抑制作用,并强调了Bcor剂量不足对MDS发生发展的影响。
Shiro Tara, et al. Bcor insufficiency promotes initiation and progression of myelodysplastic syndrome. Blood 2018 :blood-2018-01-827964; doi: https://doi.org/10.1182/blood-2018-01-827964
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Bcor#
46
#骨髓增生异常#
46
#骨髓增生异常综合#
37
#骨髓增生#
30
#发生发展#
47
#综合征#
37
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
65