ATVB:急性缺血性卒中止血生物标志物的意义
2019-02-13 xing.T MedSci原创
由此可见,基于目前的文献没有明确的建议可以提供止血生物标志物是急性缺血性卒中后临床结局的预测因子。然而,一些生物标志物显示出有前景的结果,并且需要大样本研究来进一步验证。
急性缺血性卒中后对患者不良临床预后风险的预测仍然具有挑战性。凝血因子的不平衡可能在这些患者的进展和预后中起重要作用。近日,心血管领域权威杂志Arteriosclerosis, Thrombosis, and Vascular Biology上发表了一篇研究文章,在该系统评价中,研究人员评估了目前关于止血生物标志物以及与急性缺血性卒中不良临床预后之间相关性的文献。
研究人员对Embase、Medline、Cochrane图书馆、Web of Science和Google Scholar进行了系统检索,确定了报告急性缺血性卒中后止血生物标志物和临床结果的研究。如果在症状出现后72小时内收集血样,则认为研究符合条件。此外,应使用残疾评分(Barthel指数或改良Rankin量表)评估临床结局。纳入研究的方法学质量用修订版的诊断准确性研究质量评估调查表进行评估。
共有80篇文献被阅读全文,41项研究被认为符合纳入标准,报告了37种不同的止血生物标志物。没有一种生物标志物可用于预测急性缺血性卒中患者的不良临床结局。
由此可见,基于目前的文献没有明确的建议可以提供止血生物标志物是急性缺血性卒中后临床结局的预测因子。然而,一些生物标志物显示出有前景的结果,并且需要大样本研究来进一步验证。
原始出处:
Samantha J. Donkel,et al.Prognostic Hemostasis Biomarkers in Acute Ischemic Stroke A Systematic Review.ATVB.2019.https://www.ahajournals.org/doi/10.1161/ATVBAHA.118.312102
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#缺血性#
46
#TVB#
45
#缺血性卒#
35
#标志物#
40
#止血#
31
#生物标志#
24
#生物标志#
23
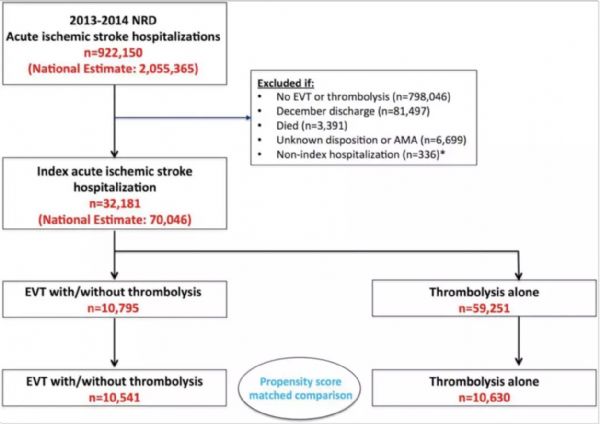
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
45