Int J Oral Sci:活动性根尖性牙周炎的不同阶段,骨重塑活性也不同
2020-04-06 MedSci原创 MedSci原创
骨骼重塑通过骨骼形成和骨骼吸收来贯穿人类的寿命。在颅面区域,下颌骨是咬和咀嚼的主要力量,一旦治疗不及时被感染的牙髓就容易导致周围骨丧失,即根尖周炎,在此期间,根尖会发生骨吸收孔至顶骨区域。尽管常规的根
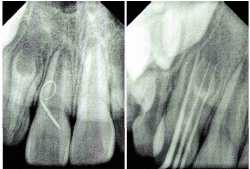
骨骼重塑通过骨骼形成和骨骼吸收来贯穿人类的寿命。在颅面区域,下颌骨是咬和咀嚼的主要力量,一旦治疗不及时被感染的牙髓就容易导致周围骨丧失,即根尖周炎,在此期间,根尖会发生骨吸收孔至顶骨区域。尽管常规的根管治疗(RCT)可以消除大部分感染,但是由于牙髓未完全清除而导致的慢性根尖性牙周炎以及随后的微渗漏将变得难治且更具挑战性,因此几乎没有专门研究此过程作为大鼠模型中的骨骼重塑问题。
因此,为了研究由于不完全清洁感染的牙髓和体内微裂而导致的慢性和难治性根尖性牙周炎,我们通过密封残留的坏死牙髓并引入有限的唾液建立了改良的大鼠渐进性根尖周炎的大鼠模型,该模型模拟了渐进性根尖周炎如在慢性和难治性根尖性牙周炎的临床治疗中观察到的。
我们发现,在这种情况下,根尖周炎的骨质流失不可避免,且呈进行性,再次证实了完整而健全的根管治疗对于制止慢性和难治性根尖周炎并促进骨形成至关重要。有趣的是,此模型的时程研究表明,在此模型中,在根尖周炎的初始阶段,骨骼重塑得到了增强,而随后的成骨细胞数量增加,骨塑形得到了降低。提示病理性根尖微环境在某种程度上保留了其硬组织形成能力,但受到干扰。
希望我们的发现可以为今后根尖性牙周炎相关的骨丢失的骨再生治疗提供见识。
原始出处:
Ruoshi Xu, Daimo Guo, et al., Disturbed bone remodelling activity varies in different stages of experimental, gradually progressive apical periodontitis in rats. Int J Oral Sci. 2019 Sep; 11(3): 27.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oral#
26
#活动性#
29
#骨重塑#
34
#牙周#
33