PNAS:核受体调节自闭症发生
2018-03-15 海北 MedSci原创
海马的齿状回(DG)是一个层状脑区域,该区域神经发生在胚胎发育早期开始,并持续到成年。已有的研究表明,DG区域的神经发生缺陷似乎与自闭症谱系障碍(ASD)样行为的发生有关。
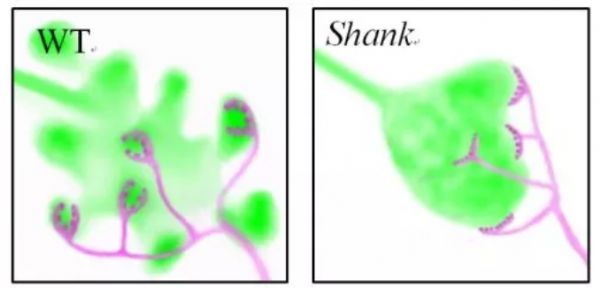
海马的齿状回(DG)是一个层状脑区域,该区域神经发生在胚胎发育早期开始,并持续到成年。已有的研究表明,DG区域的神经发生缺陷似乎与自闭症谱系障碍(ASD)样行为的发生有关。最近,肝X受体β(LXRβ)被发现可以作为参与层状CNS结构发育的重要转录因子,但至今为止,我们对其在DG发育中的作用还知之甚少。
第三军医大学的研究人员发现,在小鼠中,LXRβ的缺失能够导致DG发育不全,包括祖细胞形成和颗粒细胞分化的异常。研究人员还发现,在LXRβ缺失的小鼠中,Notch1(祖细胞自我更新的重要介质)的表达有所减少。另外,小鼠中LXRβ的缺失会导致类似自闭症的行为,包括异常的社交互动和重复行为。
这些数据揭示,LXRβ在协调DG内神经祖细胞的及时分化过程中发挥了核心作用,由此可能解释其与LXRβ缺陷小鼠发生自闭症相关行为的关系。
原始出处:
Yulong Cai et al. Liver X receptor β regulates the development of the dentate gyrus and autistic-like behavior in the mouse. Proceedings of the National Academy of Sciences, 2018; 201800184 DOI: 10.1073/pnas.1800184115
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PNAS#
0
#核受体#
29
#自闭#
21
学习一下谢谢
70
好
53