Circulation:ADCY9基因型对Anacetrapib临床疗效的影响
2019-09-18 MedSci MedSci原创
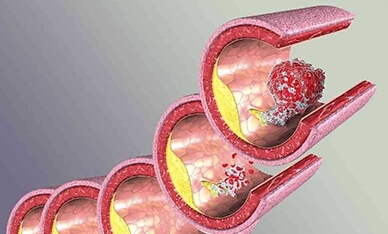
既往研究提示临床对胆固醇酯转移蛋白(CETP)抑制剂治疗的反应因ADCY9基因型的不同而不同。随机对照(REVEAL)试验证实了CETP抑制剂安塞曲匹(anacetrapib)在动脉粥样硬化性疾病患者中的临床疗效。在本研究中,研究人员对REVEAL试验中ADCY9基因型对安塞曲匹治疗的反应性的影响进行评估。接受阿托伐他汀强化治疗的稳定动脉粥样硬化血管病患者,每天服用100mg安塞曲匹或安慰剂。主要
接受阿托伐他汀强化治疗的稳定动脉粥样硬化血管病患者,每天服用100mg安塞曲匹或安慰剂。主要结点是安塞曲匹对大血管事件(冠状动脉死亡、心肌梗死、冠状动脉血管重建或假性缺血性中风的复合事件)的影响与ADCY9基因rs1967309位点基因型之间的相关性。
共19210位测定了基因型的个体。在中位4年的随访期内,2504位(13.0%)首次出现大血管事件:实验组和对照组分别有1216位(12.6%)和1288位(13.4%)。ADCY9基因型与安塞曲匹对大血管事件风险的降低比例无显著差异:基因型为GG型、AG型和AA型个体的风险比(HR)分别为0.92、0.94和0.93。此外,ADCY9基因型与安塞曲匹对各血管事件和血脂水平的影响均无相关性。
REVEAL试验是迄今为止规模最大的评估ADCY9药物基因相互作用的研究。其分析结果不支持ADCY9基因型与CETP抑制剂安塞曲匹临床疗效具有相关性的假设。
原始出处:
Jemma C. Hopewell, et al.Impact of ADCY9 Genotype on Response to Anacetrapib.Circulation. 2019;140:891–898
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#TRA#
30
#TRAP#
38
#ACE#
32
#临床疗效#
29
#ANA#
33
#基因型#
31
谢谢梅斯提供这么好的信息,学到很多
45