J Clin Oncol:奥秘皆在细微处:诊断治疗间期与新诊断弥漫大B细胞淋巴瘤预后相关
2018-05-07 李皓静 肿瘤资讯
长久以来,如何提高肿瘤临床试验结论的科学性和普适性备受关注。以往,研究者往往通过严密的试验设计、严谨的知情同意条款和科学的分析来控制偏倚。美国梅奥诊所学者Maurer等的研究结果发现,临床试验中人们甚少关注的诊断治疗间期与预后显着相关,该研究结果近日发表于JCO杂志上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



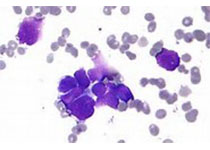
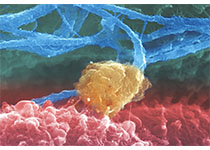
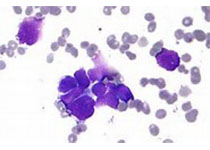




#细胞淋巴瘤#
30
#新诊断#
27
#Oncol#
32
#诊断治疗间期#
39
#B细胞#
42
#诊断治疗#
33
学习谢谢分享
79
学习了 非常感谢
92
阅
92
厉害了我的哥
77