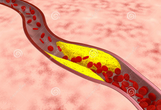
Stroke:基底动脉斑块患者,斑块内出血与急性梗死的关系
2015-09-25 phylis 译 MedSci原创
背景和目的:高分辨磁共振(HRMRI)是检测病态动脉壁的理想方法,因为HRMRI是一种无创并且组织特征区分能力较高的一种检查方法。这篇研究旨在评估应用HRMRI检测基底动脉(BA)动脉粥样硬化患者的斑块内出血的发生情况及其临床相关性。 方法:研究人员分析了74名患者(45名有症状,29名无症状的患者)的HRMRI以及临床数据,所有受试者存在超过50%的BA狭窄。在磁化强度预备梯度回波序列(MPRA
背景和目的:高分辨磁共振(HRMRI)是检测病态动脉壁的理想方法,因为HRMRI是一种无创并且对组织特征区分能力较高的一种检查方法。这篇研究旨在评估应用HRMRI检测基底动脉(BA)动脉粥样硬化患者的斑块内出血的发生情况及其临床相关性。
方法:研究人员分析了74名患者(45名有症状,29名无症状的患者)的HRMRI以及临床数据,所有受试者存在超过50%的BA狭窄。在磁化强度预备梯度回波序列(MPRAGE)上,BA斑块高信号强度是相邻肌肉信号强度超过150%的区域。分析BA斑块区域存在IPH和临床表现的关系。
结果:HRMRI显示有30名患者存在IPH(42.3%,24个有症状,6个无症状)。MR阳性的IPH组的症状性损伤比MR阴性组患者更普遍(80% VS 48.8%)。并且,与低度狭窄组相比,高度狭窄组MR预测IPH的发生更普遍。与IPH患者MRRAGE阴性组相比,IPH患者MRRAGE阳性的患者发生急性局灶性卒中的RR值为1.64。
结论:HRMRI显示BA斑块区域存在IPH非常普遍,并与急性卒中相关。
原文出处:
Yu JH, Kwak HS, Chung GH,et al.Association of Intraplaque Hemorrhage and Acute Infarction in Patients With Basilar Artery Plaque. Stroke. 2015 Aug 25.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#基底动脉斑块#
39
#斑块#
39
#基底动脉#
40
#斑块内出血#
41