J Appl Microbiol:鲍曼不动杆菌产生的凝集素或可有效抗菌及抗肿瘤
2018-04-10 MedSci MedSci原创
凝集素是一种非免疫原性糖蛋白,主要从主要植物来源的leguminoase中提取。凝集素可精确识别和结合复杂细胞结合结构从而发挥各种功能。然而凝集素的生产非常昂贵,因此,在这项研究中,研究人员旨在发现凝集素新的来源,从植物来源的细菌中分离和鉴定植物凝集素,并评估其作为抗菌剂、抗生物膜和抗增殖剂的能力。 利用表型和分子检测研究了环境来源的分离物产生凝集素的能力。从具有丰富凝集素活性的分离物AB119纯
凝集素是一种非免疫原性糖蛋白,主要从主要植物来源的leguminoase中提取。凝集素可精确识别和结合复杂细胞结合结构从而发挥各种功能。然而凝集素的生产非常昂贵,因此,在这项研究中,研究人员旨在发现凝集素新的来源,从植物来源的细菌中分离和鉴定植物凝集素,并评估其作为抗菌剂、抗生物膜和抗增殖剂的能力。
利用表型和分子检测研究了环境来源的分离物产生凝集素的能力。从具有丰富凝集素活性的分离物AB119纯化凝集素,并通过SDS-PAGE和HPLC测定其分子量。这种凝集素的分子量为30 kD,用于使用早期公布的方案评估其抗菌、抗菌和抗增殖活性。
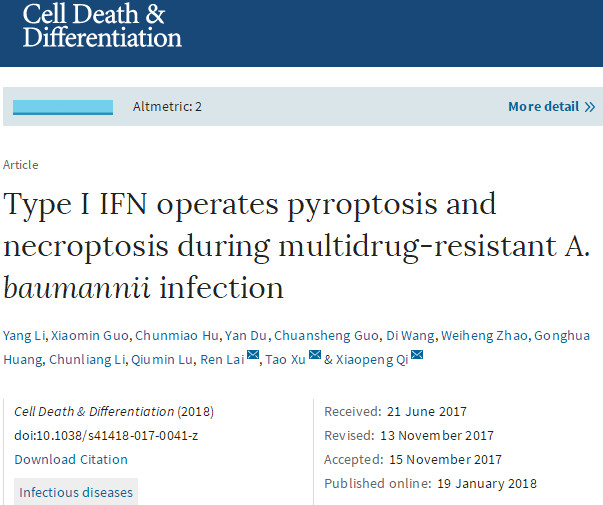
结果显示,该研究中所使用的凝集素可明显抑制生物膜的形成。在微量滴定板测定中,所有细菌物种的纯化凝集素对生物膜抑制的程度明显降低。处理24小时后,凝集素可抑制所有三种测试细菌种类的生长,并且该抗菌效果对于所有物种均是如此。使用MTT测定法测定凝集素对HeLa细胞的抗增殖作用,以10μM的IC 50 24小时对HeLa细胞的增殖具有明显的抑制作用。
综上所述,该研究结果表明,凝集素或可作为抗菌剂和抗菌膜剂用于控制多重耐药性病原体相关的感染。同时,我们的研究结果表明,凝集素也可控制肿瘤细胞增殖的能力。
原始出处:
Alyousef AA, Alqasim A, Aloahd MS. Isolation and characterization of lectin with antibacterial, antibiofilm and antiproliferative activities from Acinetobacter baumannii of environmental origin. J Appl Microbiol. 2018 Jan 19. doi: 10.1111/jam.13699.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Biol#
24
#Bio#
0
#Micro#
28
#CRO#
30
学习
61
#抗菌#
21
#鲍曼不动杆菌#
31