快速一览:2月BMJ病例报道汇总,值得一看!
2017-02-21 MedSci MedSci原创
医生每天都会遇到各种各样的疑难杂症,但还有很多临床医生都未接触过的病例,下面梅斯医学小编为大家盘点一些值得一看的病例报道,供大家学习参考,希望对大家有所帮助。【1】BMJ:这个患者为啥呼吸困难和腹部肿胀-案例报道 患者为一名50岁的女性,在数周内出现呼吸急促伴腹胀和不适而就诊。她无法平躺,由于端坐呼吸。该患者没有其他疾病以及药物治疗。进行了胸部、腹部和盆腔计算机断层扫描(CT)扫描,
医生每天都会遇到各种各样的疑难杂症,但还有很多临床医生都未接触过的病例,下面梅斯医学小编为大家盘点一些值得一看的病例报道,供大家学习参考,希望对大家有所帮助。
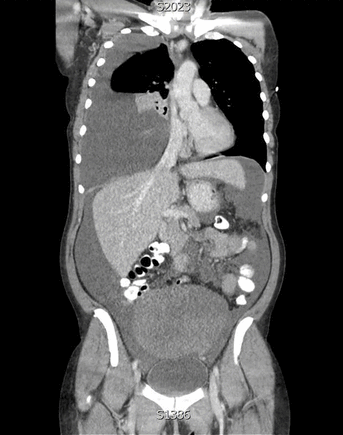
患者为一名50岁的女性,在数周内出现呼吸急促伴腹胀和不适而就诊。她无法平躺,由于端坐呼吸。该患者没有其他疾病以及药物治疗。进行了胸部、腹部和盆腔计算机断层扫描(CT)扫描,其次是活检和诊断性手术治疗。术后组织学证实为良性肿瘤。该患者CT图像有哪三个主要的影像学发现(如图1所示),这个经典的三联征相关同名诊断是啥?
图1胸部、腹部和骨盆的冠状计算机断层扫描(CT)图像
答案
CT显示右侧大量胸腔积液,导致纵隔移位和严重腹水(如图2所示)。有一个来自于骨盆的大肿块。良性卵巢纤维瘤相关的胸腔积液或腹水被称为Meigs综合征。
图2大量的右侧胸腔积液(白色箭头)引起纵隔移位(蓝箭头)。有一个来自于骨盆的大肿块(橙色箭头),这增加了恶性肿瘤或纤维瘤的可能性。也存在大量腹水(绿色箭头)
患者预后
该患者接受经腹全子宫及双侧卵巢切除手术切除了纤维瘤后,恢复良好,腹水和胸腔积液得以解决。
学习要点
Meigs综合征是由良性纤维瘤引起胸腔积液和腹水,而假Meigs综合征是原发或继发卵巢恶性肿瘤引起的。
快速转诊接受进一步调查和诊断是必需的。腹水或胸水引流可以缓解症状,但最终根治的方法是纤维瘤切除。
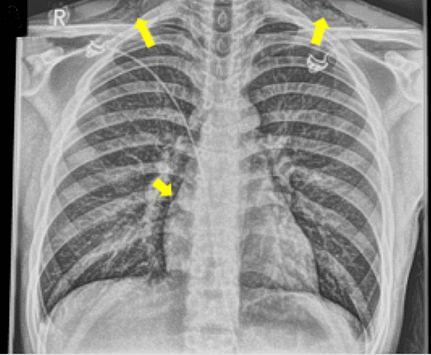
患者为一名16岁的男孩,因橄榄球比赛后出现呼吸困难和颈部肿胀疼痛而就诊。其颈部或胸部没有任何创伤。该患者有哮喘病史,最近有上呼吸道感染。沙丁胺醇不能缓解患者呼吸困难,比赛后其颈部肿胀和呼吸困难逐步恶化。X光片有何异常(如图1所示),诊断是啥?
图1 后前位胸片
答案
X光片显示纵隔内有空气。
讨论
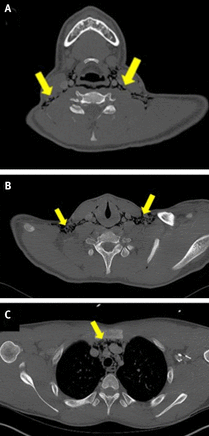
病人在描述肿胀后开始被医生关注。临床上怀疑外科性气肿,在他因脖子“噼里啪啦”的感觉而就诊时。X光片上没有看到气胸,但有一薄层空气围绕在心脏周围,颈部软组织中的空气证实为纵隔积气(如图2所示)。鼻内窥镜和CT扫描没有发现气管或食管损伤(如图3所示)。通过排除,诊断为自发性纵隔气肿。症状和体征在72小时内消退,该患者完全康复,三周后返回赛场。
图2心脏周围的空气(箭头),以及在锁骨上区软组织中的空气
图3 颈部(A,B)和胸部(C)CT图像显示空气弥漫在整个纵隔。CT扫描显示无气管或食管损伤
讨论
自发性纵隔气肿与哮喘控制不佳、上呼吸道感染等有关。该病主要影响青少年和年轻的成年人。
自发性纵隔气肿在急性发作时给予支持治疗(控制潜在的哮喘、镇痛、休息和氧疗)通常会很快缓解。不需要预防性抗生素治疗除非有食管破裂的证据。虽然通常不易复发,重点应该是对任何潜在的病因因素,如哮喘控制不佳,实现最佳控制。
患者为一名60岁的女性,在一次跌倒后颈部发生直接的创伤而入院,她的嗓音逐渐恶化,吞咽困难,颈部运动疼痛。颈部明显肿胀和青紫延续到前胸壁。对颈椎触诊无压痛。进行颈椎侧位片(如图1所示)检查,颈椎侧位片上显示了什么?
图1
答案
X光片显示巨大咽后血肿,上呼吸消化道变形和正常颈椎生理曲度消失。
轻微损伤后即可引起咽后血肿,压迫气管危及生命。咽后血肿的原因是多种多样的,病例中报告的常见原因为创伤,包括颈椎损伤、误食异物和医源性损伤。
在这个病例中,患者被认为不稳以至于刚开始不能接受CT检查,因此,急诊手术气管切开和引流血肿前进行清醒纤维支气管镜气管插管。病人没有任何骨损伤的临床证据;对棘突触诊无压痛,神经系统检查无明显异常。从咽后间隙引流出约400毫升血液,并且插入了两排引流管。术后成功地进行CT扫描(如图2所示),显示纵隔内有少量残余血肿和排除颈椎骨折。在术后九天拔除引流管,一个月后气管拔管成功。该患者从这次创伤中恢复得很好。
图2术后CT扫描在咽后间隙显示两个引流管。原位气管切开、鼻饲管插入
学习要点
咽后血肿呈现食管和气管受压、气管位置前移和颈部和前胸皮下淤血的三联征。
侧位颈部X线检查有助于确定软组织肿胀。
患者一名81岁的女性,因其食指肿胀、呈红色伴疼痛而向她的初级保健医生咨询(如图1所示)。该症状已经持续了几天。患者无发热,不记得有任何伤害。几周前,该患者出现过类似的肿胀,服用氟氯西林后肿胀有所缓解但并没有完全消除。病人既往有2型糖尿病和高血压,服用格列美脲、福辛普利、氯噻嗪、氨氯地平、阿托伐他汀。在体格检查时,发现远节指骨和远端指间关节红肿。皮肤完好无损,没有任何伤口,指间关节活动受限。病人转诊至风湿免疫科。进行血液检测,并进行诊断性穿刺术抽取受影响的关节滑液。涂片显微镜检查(如图2所示)。
图1 81岁女性红肿的手指
图2抽吸的关节液显微镜下结果
问题和回答
1.根据显微成像和病史,诊断是什么?
远端指间关节急性痛风
2.手指远端肿胀的鉴别诊断是什么?
其他需要鉴别的疾病有甲沟炎、假性痛风、急性发炎的骨性关节炎、银屑病关节炎、化脓性关节炎。
3.治疗的选择是什么?
非甾体抗炎药、秋水仙碱、口服皮质类固醇或关节皮质类固醇注射。
患者预后
该患者血清尿酸水平为510µmol/L,并且穿刺关节液检查有尿酸钠晶体(如图3所示)。该患者开始使用秋水仙碱和别嘌呤醇治疗。近五个月后,病人手指的病灶处已恢复正常(如图4所示)。
图3抽吸的关节液显微镜下结果:红细胞尿酸钠晶体
图4治疗五个月后受累手指
患者为一名62岁男性,因在轻微跌倒后肩部疼痛恶化而就诊。医生要求进行X线检查,根据患者X线检查结果(如图1所示),下一步该怎么做?
图1右肩前后位平片
答案
进行胸部和上腹部计算机断层扫描(CT)检查。肩关节X线片显示空泡肺结节,测量其大小约2厘米(如图2所示)。这最有可能是原发性肺癌,并应转诊到肺癌多学科团队就诊。
图2右肩前后位平片,右肺有空泡肺结节(红色箭头
学习要点
当看到一个孤立的肺结节,请肺癌多学科团队进行适当的进一步调查。
患者预后
病人进行胸部和腹部CT扫描以及随后进行的肺活检,发现为T2N0M0原发性肺腺癌。该患者接受手术切除,病人在两年内安然无恙。
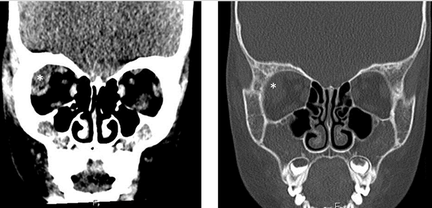
患者为5岁男孩,既往有镰状细胞病,因右眼框肿胀2天而就诊。该患者疑似眼眶蜂窝组织炎开始静脉注射抗生素治疗。
其体温正常,而且视力和眼球运动正常。计算机断层扫描(如图1所示)显示右上外侧有眼眶肿块,但没有鼻窦疾病。白细胞计数和C反应蛋白水平正常。最终诊断为眼眶外侧骨梗死,由于镰状红细胞,继发血肿。
这个疾病可以与其他急性眼眶病变如眶蜂窝织炎混淆。这对患者视力构成了潜在的威胁,由于眼眶腔室综合征,并可与颅内血肿相关。
虽然磁共振成像是诊断眼眶梗塞的最佳影像学检查方法,但由于其临床情况,该患者并未进行磁共振成像。该患者经静脉输液和全身皮质类固醇治疗后,完全恢复。
患者为一名68岁的女性,因间歇性血尿和左侧腰部疼痛6个月而就诊。
膀胱镜检查和肾脏超声检查的结果均为阴性。腹部和盆腔CT显示左侧性腺血管扩张(如图1所示)。
图1
位于主动脉和肠系膜上动脉之间的左侧肾静脉受压迫,导致静脉高压引起血尿、腰部疼痛。这种罕见的现象被称为胡桃夹综合征。对于尿路成像的超声、静脉尿路造影及膀胱镜检查正常的腰痛和血尿患者应该怀疑是否为胡桃夹综合征。
外科手术治疗包括左侧肾静脉移位或自体扩张支架的血管内治疗。如果没有严重的血尿相关贫血或盆腔剧烈疼痛,该病预后良好。
患者为一名81岁的女性,因其在右臀部发现一个10厘米的恶臭、易碎、菜花状和带蒂肿瘤(如图1所示)而到皮肤癌诊所就诊。
图1
因就诊时该患者病变被怀疑为恶性病变,所以该病灶立刻被皮肤病医生予以切除。
令人惊讶的是,在组织学分析的结果中发现该病变与发炎和刺激脂溢性角化病相一致,该病为一种良性皮肤生长性疾病,常见于成年人,并常被称为老年疣。有文献报道了脂溢性角化病的不寻常表现,包括那些已经与恶性肿瘤相混淆的临床表现。
报道本病例获得患者同意,并且主要强调临床病理相联系的重要性。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#BMJ#
20
了解了
45
好东西学习了!
60
特殊病例分享
47
特殊病历,认真学习一下。谢谢分享!
51
不错学习了,分享一下
58