STEM CELL REP:hPSC助力人工造肾
2018-02-10 海北 MedSci原创
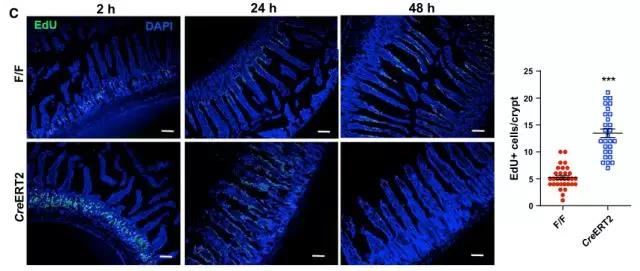
人类多功能干细胞(hPSCs)技术的发展对于我们理解肾脏发育过程和相关疾病具有很大的帮助。最近,来自曼彻斯特大学的研究人员重复地将三个基因独特的野生型hPSC系分化成为肾脏祖细胞,并观察到了初步的肾体外形态发生。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
24
#CEL#
33
#stem cell#
28
#PSC#
38
#STEM#
33
了解了解.继续关注
77