关注高血压管理 谱写防治新篇章 ——专访中南大学湘雅医院杨天伦教授
2018-09-30 导报 中华医学信息导报
近年来,随着社会老龄化及人民生活水平的不断提高,我国高血压的发病率不断升高。基层医疗机构是高血压管理的“主战场”, 其管理水平的高低将直接影响我国心血管疾病的发展趋势。目前,基层医院对患者降压达标和改善高血压控制率是高血压管理面临的主要任务,基层医院对高血压的防治还存在哪些不足?如何全面提高基层高血压的管理水平?基于这些问题,本报记者采访了中南大学湘雅医院杨天伦教授,探讨我国高血压防治存在的主要问
前言
近年来,随着社会老龄化及人民生活水平的不断提高,我国高血压的发病率不断升高。基层医疗机构是高血压管理的“主战场”, 其管理水平的高低将直接影响我国心血管疾病的发展趋势。目前,基层医院对患者降压达标和改善高血压控制率是高血压管理面临的主要任务,基层医院对高血压的防治还存在哪些不足?如何全面提高基层高血压的管理水平?基于这些问题,本报记者采访了中南大学湘雅医院杨天伦教授,探讨我国高血压防治存在的主要问题及对策。
据相关数据显示,当前我国高血压患者人数约有2.7亿。请您谈一谈,目前我国高血压的流行病学趋势?
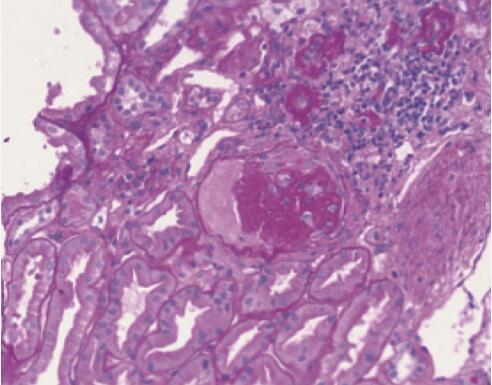
高血压是严重危害人类健康的常见心血管疾病之一,也是全球范围内的重大公共卫生问题。近年来, 随着社会老龄化及人民生活水平的不断提高,我国高血压的发病率不断升高,且呈年轻化的趋势。目前,我国高血压患病人数约达2.7亿,包括卒中、冠心病、心力衰竭等在内的严重并发症,其致残和致死率较高,已成为我国家庭和社会的沉重负担。
然而,高血压可防可控, 有研究表明,降压治疗可降低卒中发病风险35%~40%,降低心肌梗死发病风险20%~25%,降低心力衰竭风险超过50%。因此, 预防和控制高血压,是遏制我国心脑血管疾病的核心策略。
基层医疗机构是高血压管理的“主战场”,但是却存在诸多问题。请您谈一谈,我国基层心血管学科医师在高血压管理上存在哪些问题或不足?
基层医疗机构(社区卫生服务中心、乡镇卫生院、村卫生室等)是高血压管理的“主战场”,其管理水平的高低将直接影响我国心血管疾病的发展趋势。但是,基层医疗机构对高血压的管理仍存在诸多不足。
一方面,患者对高血压的认知程度较低,这就需要基层医师不断加强对患者的健康教育。根据患者具体情况,与患者共同讨论需要改善的生活方式,指导患者健康饮食及正确测量血压等,帮助患者做好高血压综合干预管理,严格控制血压水平,预防并发症的发生。另一方面,我国基层医师的诊疗理念和综合能力还需进一步加强。目前,我国正推进基层慢性病管理政策,大力开展各类慢性病防治知识培训活动,但是,很多基层医师对该类培训仍缺乏一定的关注度。因此,我们不仅要加强基层医师高血压防治的理论与技能培训,指导其临床实践,进行合理诊疗, 更要注重基层医师诊疗理念和综合能力的培养及完善,使基层医院的疾病管理水平得到全面的提高。在培训活动的开展方面,基层医院还需要进一步完善培训计划,合理安排内容及正确选择媒体方式。
指南对高血压的诊断方法、危险因素评估、治疗策略、综合干预、转诊原则及随访管理等内容进行了详细介绍。具体内容的可操作性、实用性较强,为基层高血压的防治管理提供了简单易行的治疗方案;而药物治疗的推荐则为促进基层医疗卫生机构与上级医院在高血压管理上的同质化发展奠定了基础。
指南提出,高血压治疗的目标是血压达标,血压尽早达标有利于减少心脑血管事件,这就要提高高血压治疗率和控制率。因此,基层医院对患者降压达标和改善高血压控制率是高血压管理面临的主要任务。未来几年,我们的目标是将高血压患者的认知率、服药率、控制率提高到30%~35%以上,对患者进行综合干预管理,严格控制患者24 h血压水平,以防发生卒中、冠心病等并发症。基于该目标,基层医院既要建立规范化的高血压管理体系,包括高血压的筛查、诊断、治疗、随访等流程规范,也可以参考指南中简便易行的管理方法,使用安全有效的降压药进行合理诊疗;还要进一步加强基层医院对高血压管理技能的培训,促进基层医师的经验交流与学习,共同提高高血压的防治能力,努力实现降压达标。
作为ACTIVE项目的核心专家,您打算如何将全国优秀心内科的先进理念和技术带到基层?
首先,我们会加强对基层医院心血管疾病防治技能的培训,将组织全国各医院心内科临床经验丰富、专业技能水平高、擅长演讲的优秀医师,到各地区基层医院进行心血管疾病诊疗理论与技能的巡讲,以指导基层医师临床诊疗实践,提高疾病的诊治能力。同时,我们也会注重培养医师严谨求实的行医理念,指导基层医师对心血管疾病进行诊断分析,把握寻根溯源、因病施治的原则,控制疾病的发生发展,从而达到标本兼治。
此外,锻炼基层医师对患者合理转诊、及时会诊、随访管理的能力也至关重要。心血管科医师如遇到起病急、症状重、怀疑继发性高血压以及多种药物无法控制的难治性高血压患者,要及时采取双向转诊、网络会诊等处理措施,转诊后2~4周基层医师应主动随访,了解患者在上级医院的诊断结果或治疗效果,达标者可恢复常规随访。这样才能对患者进行早发现、早治疗,及时控制病情发展,使更多患者受益。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#高血压管理#
32
#专访#
21
#新篇章#
30
#血压管理#
39
#湘雅#
32
学习了
57