ESC 2015:未来心血管热点领域——P4医学、斑块负荷、TAVR、环境污染
2015-09-01 MedSci MedSci原创
Brugada:P4医学将走入主流西班牙心律失常专家Brugada教授指出,与传统医学的被动性反应相悖,将来医学将向P4医学发展,即对疾病更有预测性(predicative),诊断治疗的个体化(personalized),整体人群的参与(participative)以及对疾病的预防(preventive)。而人们更是将透彻地认识更多心律失常的分子机制,掌握更多的先进技术如无创起搏器甚至将来将出现的
Brugada:P4医学将走入主流
西班牙心律失常专家Brugada教授指出,与传统医学的被动性反应相悖,将来医学将向P4医学发展,即对疾病更有预测性(predicative),诊断治疗的个体化(personalized),整体人群的参与(participative)以及对疾病的预防(preventive)。而人们更是将透彻地认识更多心律失常的分子机制,掌握更多的先进技术如无创起搏器甚至将来将出现的生物起搏器。从解剖到生理,从细胞学到分子学,人类将史无前例地解开疾病的秘密。

从易损斑块到斑块负荷,重塑斑块概念
Vrints教授挑战了冠心病的易损斑块概念。他认为,随着影像手段的发展,以往越来越多的急性冠脉综合征由斑块的腐蚀导致,而将来的工作重点也将由稳定斑块过度到降低斑块负荷,这就需要更早的影像学及基因谱的诊断方法。
TAVR在2025年将成为主导性技术
TAVR的创始人Cribier教授大胆地设想在2025年,TAVR将取代大部分主动脉瓣膜的外科手术治疗。TAVR的适应证将进一步扩展.而如二尖瓣等其他瓣膜的介入技术也向外科手术提出了更大的挑战。
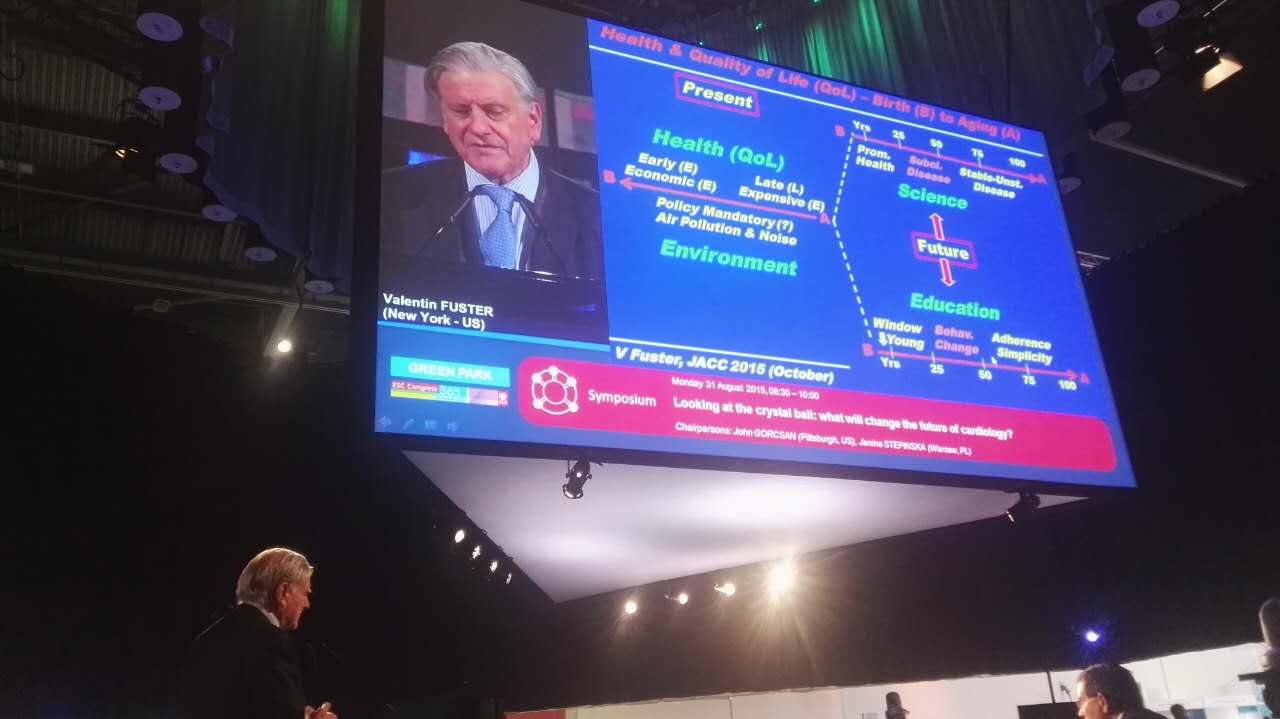
环境污染对心血管危害巨大
《美国心脏病学会杂志》(JACC)主编Fuster探讨了目前环境污染和CAD的沉重话题。即使在美国,降低pm 2.5水平也能降低每年8000例住院及减少1亿美元的医疗开支。而将来的心血管防治工作,更要将科学进展与教育并进,使疾病在亚临床状态即得到控制。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







感谢作者分享
21
#AVR#
29
#斑块#
27
#污染#
26