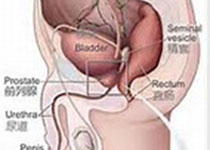
JAMA Oncol:3期转移性去势抵抗前列腺癌临床试验中患者角度的副作用事件评估
2019-11-03 Alex Yang MedSci原创
癌症临床试验中标准副作用事件(AE)报道依赖于临床医生分级,先前的研究已经表明了依赖于临床医生的分级能够导致低估有症状的AEs。行业赞助商正在试行美国国家癌症研究所患者报告的副作用事件通用术语标准结果版本(PRO-CTCAE),该标准的目的是使患者能够自我报告有症状的AEs,从而提高有症状AEs检测的质量。最近,有研究人员在一个预先指定的3期COMET-2试验中评估了PRO-CTCAE的可行性情况
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#副作用#
29
#去势抵抗前列腺癌#
26
#Oncol#
25
#转移性#
27
谢谢梅斯分享这么多精彩信息
46
前列腺癌相关研究,学习了,谢谢梅斯
34