J Endod:布洛芬和醋氨酚与鼻内用酮咯酸(Sprix)对未加处理的牙髓疼痛模型的止疼效果比较:一项随机双盲试验
2019-03-03 lishiting MedSci原创
早先,酮咯酸只能通过静脉注射和肌肉注射给药。现在有鼻内给药的剂型,大大方便患者能够自行给药。这篇研究的目的是为了评估鼻内用酮咯酸(Sprix; Egalet US Inc, Wayne, PA)与布洛芬/醋氨酚联合应用对未经处理的存在中到重度疼痛和有症状根尖周炎患者的急性疼痛模型的止疼效果比较。
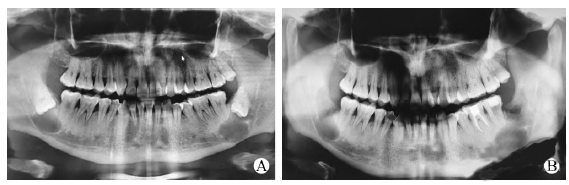
早先,酮咯酸只能通过静脉注射和肌肉注射给药。现在有鼻内给药的剂型,大大方便患者能够自行给药。这篇研究的目的是为了评估鼻内用酮咯酸(Sprix; Egalet US Inc, Wayne, PA)与布洛芬/醋氨酚联合应用对未经处理的存在中到重度疼痛和有症状根尖周炎患者的急性疼痛模型的止疼效果比较。研究纳入70名存在中到重度疼痛的患者,牙髓诊断为有症状的不可逆牙髓炎或牙髓坏死,尖周诊断为有症状的根尖周炎。将患者随机分为2组,给予31.5 mg鼻内用酮咯酸和安慰剂胶囊或给予1000 mg醋氨酚/600 mg布洛芬胶囊和模拟鼻腔喷雾。给药后,每隔15分钟由患者通过VAS量表记录疼痛评分直至240分钟。记录内容包括:50%疼痛减轻的时间、疼痛减轻的第一反应时间和有意义的疼痛减轻时间,随后分析数据。结果显示,疼痛水平维持相对平稳的一段时间后,在定量给药后的120分钟才出现疼痛减轻的记录。2组间50%疼痛减轻的时间、疼痛减轻的第一反应时间和有意义的疼痛减轻时间之间没有显著性差异。结论:鼻内用酮咯酸的效果与1000 mg醋氨酚/600 mg布洛芬联合应用没有明显差异。鼻内用酮咯酸为临床医师提供了一种非
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#酮咯酸#
25
#牙髓#
21
好
72
谢谢分享学习
61
#双盲#
33
好
60
好
62
谢谢了,学习
53
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
17
梅斯里提供了很多疾病的模型计算公式,赞一个!
20