Cancer cell:重大发现!一种代谢酶能抑制肝癌细胞的生长和扩散
2020-06-29 转化医学网 转化医学网
肝癌由于其发病原因的复杂性,治疗难度很大。目前还没有针对性的、有效的肝癌治疗方法。而近日,美国的一项新研究发现了一种酶能够阻止并抑制肝癌快速生长和扩散的代谢过程,这一发现可能会在未来为肝癌提供新的疗法
肝癌由于其发病原因的复杂性,治疗难度很大。目前还没有针对性的、有效的肝癌治疗方法。而近日,美国的一项新研究发现了一种酶能够阻止并抑制肝癌快速生长和扩散的代谢过程,这一发现可能会在未来为肝癌提供新的疗法。
这项研究由美国桑福德伯纳姆普利贝斯医学研究所(Sanford Burnham Prebys)的兼职教授,威尔康奈尔医学院(Weill Connell Medicine, WCM)的病理学和实验室医学教授Jorge Moscat博士领导,并于6月25日在线发表在《癌细胞》上。题目为“PKCλ/ι Loss Induces Autophagy, Oxidative Phosphorylation, and NRF2 to Promote Liver Cancer Progression”
美国每年约有27000人死于肝癌。这种癌症与非酒精性脂肪肝(NAFLD)有关,NAFLD是一种肝脏中储存过多脂肪的疾病,其在美国的发病率呈上升趋势,它反过来又与肥胖、糖尿病和代谢综合征等更常见的疾病有关。
这项研究的通讯作者,Jorge Moscat博士说:“与其他类型的癌症相比,肝癌的治疗并不是特别有效,这是一种毁灭性的疾病。肝癌的起源与许多基因突变有关,但科学家们还没有完全了解哪些基因突变是导致癌症的直接原因。这些突变似乎在推动疾病发展中起着关键作用,但它们很难被阻断或减缓,这就是目前我们缺乏针对性的、有效的肝癌治疗方法的原因。”
这项研究表明,在小鼠和人肝癌细胞中,低水平的蛋白激酶C(PKC)λ/i与肿瘤的侵袭性有关,并且该蛋白具有抑癌作用。研究人员还描述了PKCλ/i直接阻断并抑制肿瘤生长的代谢途径。
目前,Moscat的研究团队正致力于寻找使癌细胞独立于其基因突变来源的生存和生长途径,这被称为非致癌脆弱性(non-oncogenic vulnerabilities)。先前在他的实验室中,对非致癌脆弱性的研究表明,PKCλ/i在结直肠癌中起到抑癌作用。
在这项研究中,Moscat描述了PKCλ/i的丢失是如何促进肝肿瘤增殖的。为了获得生存所需的燃料,肝癌细胞激活了燃烧葡萄糖和脂质的代谢过程。这两个过程激活了NRF 2蛋白,NRF 2蛋白调控特定基因产物的表达,从而驱动肝细胞增殖和肿瘤生长。
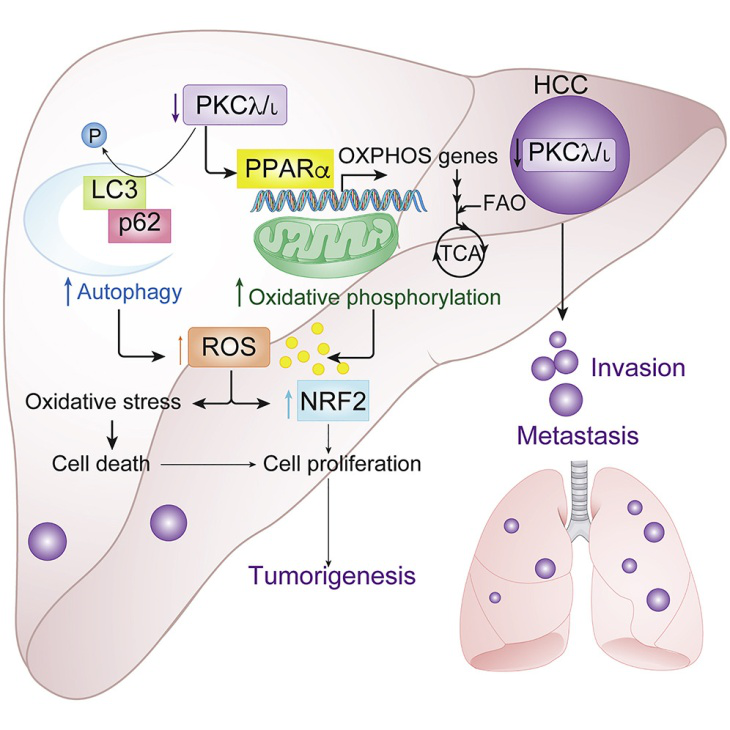
研究人员发现PKCλ/i可以阻止肝癌细胞利用这些代谢过程。因此,当肿瘤失去PKCλ/i时,它们就会变得具有攻击性。
研究小组通过研究患有肝癌的老鼠发现:当去除PCKλ/i时,癌细胞能够快速增殖。他们还观察了这些小鼠的代谢过程和NRF2蛋白的激活过程。
Moscat和他的团队还研究了明尼苏达州梅奥诊所的271份人肝癌样本,发现PKCλ/i在侵袭性癌症中的表达明显降低。此外,研究人员对139个肝癌患者的手术切除组织进行了研究,发现非肿瘤组织中PKCλ/i的低表达与恶性肿瘤的侵袭性有关。
Moscat说:“我们认为PKCλ/i标志着这种疾病的侵袭性。我们认为,这种激酶水平较低的患者更容易患上侵袭性更强的癌症。”
在未来的研究中,Moscat和他的实验室将要探究,是否可以靶向PKCλ/i或其激活的代谢途径作为潜在的治疗方法。
Moscat表示:“肝癌是一种可怕的疾病,但如果我们能通过药物调节激酶或代谢途径,我们就有可能开发出新的治疗方法。”
原始出处:
YotaroKudo,et al. PKCλ/ι Loss Induces Autophagy, Oxidative Phosphorylation, and NRF2 to Promote Liver Cancer Progression. Cell, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肝癌细胞#
42
#重大发现#
45
#CEL#
22
#Cell#
28
#cancer cell#
27
#癌细胞#
29
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
30