Clin Oral Investig:常规根管治疗联合光动力疗法可更好的促进根尖周愈合
2017-11-09 MedSci MedSci原创
本项随机对照试验旨在光动力疗法(PDT)对临床成功(根尖周愈合)和原发性牙髓感染微生物的有效性。将伴有下颌磨牙根尖周炎的32名患者随机分为对照组(化学机械清创[CMD];n = 16)和PDT(CMD + PDT;n = 16)两组。两组中的所有牙齿在最后的封闭之前用氢氧化钙根管内内给药7天。第3个月和6个月随访进行X光片检查。按照根尖指数(PAI)评估根尖周愈合。基线时期,CMD之后联合或不联合
本项随机对照试验旨在光动力疗法(PDT)对临床成功(根尖周愈合)和原发性牙髓感染微生物的有效性。
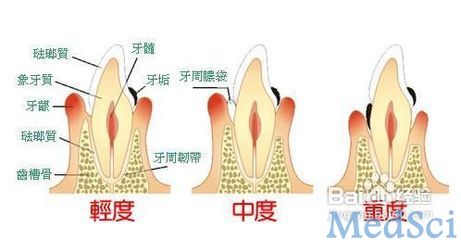
将伴有下颌磨牙根尖周炎的32名患者随机分为对照组(化学机械清创[CMD];n = 16)和PDT(CMD + PDT;n = 16)两组。两组中的所有牙齿在最后的封闭之前用氢氧化钙根管内内给药7天。第3个月和6个月随访进行X光片检查。按照根尖指数(PAI)评估根尖周愈合。基线时期,CMD之后联合或不联合PDT后,根管充填前获取样本以确定37个微生物类群的感染的频率和水平。
结果显示,随着时间的推移,两组的PAI评分均明显降低,不过第6个月随访时,PDT组的愈合评分明显优于对照组(p <0.05)。在基线时,所有样本中最普遍的存在的微生物是白色念珠菌(46.9%),肺炎链球菌(31.2%),普雷沃氏菌(28.2%),普雷沃氏菌(28.1%)和消化链球菌(25%)。两组中大多数微生物会随着时间的推移而减少,且在随访期间微生物的频率和水平无明显组间差异。在治疗后3个月,两组白色念珠菌和肺炎双球菌的检出率仍然较高。
常规牙髓治疗联合或不联合PDT均可有效减少微生物的量,促进根尖周愈合。然而,在6个月的随访中,辅助应用PDT根尖周愈合的状况更佳。因此,使用PDT辅助常规治疗根尖牙周炎可更好的促进根尖周愈合并降低微生物的水平。
原始出处:
de Miranda RG, Colombo APV. Clinical and microbiological effectiveness of photodynamic therapy on primary endodontic infections: a 6-month randomized clinical trial. Clin Oral Investig. 2017 Nov 7. doi: 10.1007/s00784-017-2270-4.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oral#
33
#EST#
0
#根管#
45
#光动力#
29
学习学习学习
90