NEJM:鼻腔插入磁铁的后果-病例报道
2017-10-26 xing.T MedSci原创
该患者在全身麻醉后被带到手术室进行手术取出磁铁。磁铁是通过在鼻子两侧放置的家用磁铁从鼻中隔上提出来的。磁铁所造成了鼻中隔软骨挤压和粘膜软骨膜的侵蚀。在受创伤的组织表面放置粘连屏障,并使用夹板10天。
患者为一名11岁的男孩,因其鼻子两侧插入磁铁后6小时被送到急诊室就诊。该患者无法取出磁铁,出现鼻出血和剧烈疼痛症状。
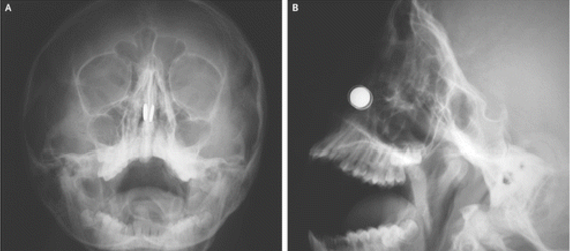
鼻腔检查显示有粘液和结痂的血块。面部拍片显示两圆盘状异物贴在鼻中隔相同的水平(图A显示冠状面,图B显示矢状面)。吸引在鼻部的磁铁需要紧急移除,因为它们可以压缩鼻中隔粘膜,导致坏死和鼻中隔穿孔。由于强烈粘连,急诊室人员试图移除磁铁并未成功。
该患者在全身麻醉后被带到手术室进行手术取出磁铁。磁铁是通过在鼻子两侧放置的家用磁铁从鼻中隔上提出来的。磁铁所造成了鼻中隔软骨挤压和粘膜软骨膜的侵蚀。在受创伤的组织表面放置粘连屏障,并使用夹板10天。
随访6个月后,先前暴露的软骨被健康的鼻粘膜所覆盖。
原始出处:
Kadir C. Kazikdas,et al. Button Magnets in the Nasal Cavity.N Engl J Med 2017; http://www.nejm.org/doi/full/10.1056/NEJMicm1708934
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习
47
#鼻腔#
45
学习了.谢谢
61
学习了新知识
60
谢谢分享
49