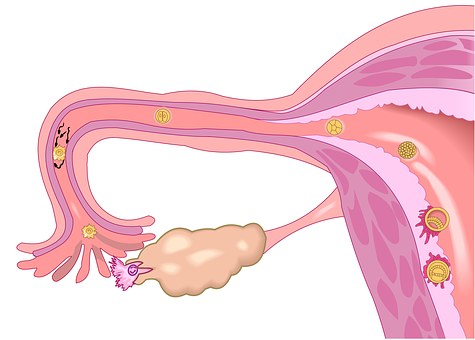
CLIN CANCER RES:针对卵巢癌TP53“热点突变”及特异性新抗原的T细胞反应
2018-11-21 MedSci MedSci原创
CLIN CANCER RES近期发表了一篇文章,评估转移性卵巢癌患者肿瘤中针对自体体细胞突变新抗原的T细胞反应。
CLIN CANCER RES近期发表了一篇文章,评估转移性卵巢癌患者肿瘤中针对自体体细胞突变新抗原的T细胞反应。
作者扩增了切除后的转移性卵巢癌病灶中的肿瘤浸润淋巴细胞(TIL),通过全外显子和转录组测序分析鉴定自体体细胞突变。在自体抗原呈递细胞中表达所有突变的新表位,然后与TIL共培养。IFNγ分泌或41BB的上调表明存在T细胞反应。研究对 7名转移性卵巢癌患者进行了评估,5名患者出现对突变新抗原显着的T细胞反应,且通过与野生型序列比较,最小表位的鉴定,人白细胞抗原(HLA)限制性因素和新抗原特异性T细胞受体等得到验证。突变的新抗原受HLA-B,-C,-DP,-DQ和/或-DR等位基因的限制,且来自每个患者独有的随机体细胞突变。作者发现两个不同患者肿瘤表达的TP53 "热点"突变(c.659A> G; p.Y220C和c.733G> A; p.G245S)均具有免疫原性。
原始出处:
Drew C. Deniger, Anna Pasetto, et al. T-cell Responses to TP53 “Hotspot” Mutations and Unique Neoantigens Expressed by Human Ovarian Cancers. CLIN CANCER RES. November 2018 doi: 10.1158/1078-0432.CCR-18-0573
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#T细胞反应#
43
#热点突变#
0
#特异性#
40
#p53#
38
#TP53#
43
#抗原#
0
学习了谢谢
67