【一般资料】
患者,男,43岁
【主诉】
因“突发胸痛6h”由外院转入。
【现病史】
其于当地医院诊断为急性广泛前壁心肌梗死。并于发病后4h在当地医院行冠状动脉造影,术中示左前降支自近段第一对角支发出以远完全闭塞,第一对角支开口60%以上狭窄,左回旋支近段60%以上狭窄,前向血流TIMI2级,右冠状动脉广泛弥漫性病变,于左前降支开通后先后置入2.5mm×18.0mm、2.5mm×29.0mmFirbird支架2枚。但在介入手术中患者自诉胸痛及心前区憋闷感较前明显加重,持续心电监测示血压进行性下降,最低时仅75/43mmHg,高度怀疑因冠状动脉破裂引发,但此时并未见明显造影剂外泄征象(图1)。予去甲肾上腺素0.45μg?kg-1?min-1血压维持,并于其胸壁左乳头下第五肋间尝试利多卡因局部麻醉,使用sliding法穿刺植入单矛引流软管1根,经约10min开放引流条件下,其引流物仅150ml鲜血。此时其血压仍需要较大剂量去甲肾上腺素维持,生命体征仍不稳定,患者自诉症状未改善,且觉穿刺位点处疼痛剧烈。遂于术中经左侧股动脉植入主动脉内球囊反搏(IABP),经1:1反博后循环仍未见好转,持续监测血压仍呈下降趋势。因当地无继续治疗条件长途转入我科,携入悬浮少白红细胞4个单位。

图1 术前外院造影
a:显示为前降支完全阻塞; b:显示为经开通后支架植入; c:完全开通后造影确认无造影剂外渗。
【体格检查】
入院后听诊心音低钝、遥远。
【辅助检查】
完善床边心脏超声心动图提示:左室前壁心肌活动明显减弱,但心肌异常增厚,见一漂浮管似位于心脏表面,前端与心脏浅表关系紧密,估测此时左室射血分数(EF)约46%。床边心电图提示窦性心律,多导联ST段抬高,提示广泛前壁心肌梗死。该患者入院后收住CICU,但体征仍不稳定,呈休克貌,床边原有去甲肾上腺素用量渐增大,最高约0.9μg?kg-1?min-1,血压仍难以维持,最低81/43mmHg。此时经原发症状初始已有6h。
【初步诊断】
经评估后患者无内科保守治疗指征,
【治疗】
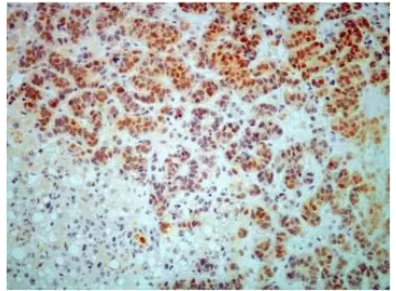
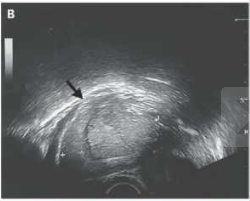
遂急诊在全身麻醉、非体外循环下行“开胸探查及心脏修补术”。术前麻醉常规于右侧颈内静脉植入漂浮导管一根,此时测得心排达6.1L/min,SVO2为51%,但经计算体循环阻力仅为760(dyne×sec)/cm5。术中开胸见心包内实无明显血液积存,但心肌肿胀剧烈,打开心包后见心脏呈整体扩张、肿胀样改变。左室活动较差,见单矛引流软管刺入心脏左室表面,局部破裂,心脏伤口表面仍见新发出血(图2)。取用约3×3cm自体心包补片沿伤口外周连续缝合,将心脏表面穿刺点破损处局部修补加以止血。此后原拟关胸,但在合拢胸骨时血压波动异常,反复有快速室性心律失常发生,心率170-180次/min,经食道超声(TEE)证实其存SAM(systolicanteriormotion)征(图3),快速补充血浆,使用少量β受体阻滞剂静脉注射,减低血管活性药物用量后缓解,但此时心肌仍较为肿胀,遂延迟关胸。并将左西孟旦剂量调整至0.5μg?kg-1?min-1,此后监测其心排呈渐进性上升趋势,心率逐渐下降至110次/分钟,于调整后2h测得床边心排量为3.3L/min,SvO2为45%。循环逐渐趋于稳定。于术后第5天顺利撤除IABP,并行延迟关胸术,此时见心脏体积已明显回缩,接近正常大小,但前壁收缩幅度仍不佳。经阶段调整返回普通病房。出院前患者复查彩超测得左心室射血分数(LVEF)36%。

图2 术中所摄重度肿胀心脏

图3 术中经食道超声证实SAM征表现
【讨论】
近年来,随着心脏介入手术的广泛开展,因导管及器械导致心肌冠状动脉穿孔引起的因积血引发急性心脏压塞并不少见,且因现代各中心外科水平的提升,开展急诊手术的速度衔接较快,国内已有诸多成功案例报道。临床判断心包填塞的早期症状多后,多立即进行心包穿刺引流等紧急措施进行缓解。但在本例患者中,我们术中探查并未见到常见的因冠脉穿孔引发的积血导致心包填塞的状况,实属罕见。临床报道急性心脏压塞多由于冠状动脉穿孔造成,其是PCI术中发生率较低的一种严重并发症,发生率约1%,基本诱发原因主要考虑因冠状动脉穿孔后导致密闭心包内积血导致心肌舒张功能障碍相关。其高危因素主要见穿孔大小、应用抗凝药物、球囊扩张次数等。但本例患者所特殊的,是其心包填塞的主因是心肌的高度充血性肿胀,而并非心包内积血。我们分析,其在进行PCI操作的过程中,为广泛性的心肌梗死引发,心肌梗死早期心肌水肿剧烈,且其左冠优势,心肌梗死累及范围较大,从而导致这一特殊改变。当地医院所采用的IABP措施,虽然减轻了患者心室的后负荷,但并未能及时减轻其心包对其自身的压迫,其种种迹象均与常见的心包填塞及其相似,故进行了穿刺这一操作,加重了心脏的损伤。但其没有明确的B超证据引导下进行,造成穿刺失误。在本例中我们观察到患者在术中并发了SAM现象。SAM现象即二尖瓣前叶前向运动,多见于肥厚性心肌病患者。目前认为SAM可导致左室流出道梗阻,严重者造成继发性二尖瓣关闭不全。造成机制其主要包括:文丘里效应和拖曳效应。文丘里效应,即左室流出道狭窄,血流速度加快,流出道相对负压,吸引二尖瓣前叶及腱索前向运动贴紧室间隔。为退行性瓣膜病中二尖瓣脱垂后发生的SAM所致左室流出道梗阻的主要机制。拖曳效应,即由于肥厚的室间隔使乳头肌排列紊乱,当心脏收缩时,肥厚的室间隔挤压绷紧的腱索,腱索后移,而二尖瓣叶上翘前移,迫使二尖瓣叶进入血液几乎排空的左室流出道。本例患者经术中TEE及术后彩超均并未有明确的二尖瓣病变,而导致这一现象的主要原因是因其心肌剧烈的充血及水肿导致其心肌明显增厚,呈类似肥厚性心肌病样改变,造成左室流出道的压迫,形成狭窄的假象,但通过对症治疗后尚可以纠正。这也为在诊疗本类患者人群,尤其是在血流动力学剧烈波动的情况下,提供了一个另类的诊断思路,需临床高度重视。本例患者经修补后,并未进行冠脉搭桥术,主要考虑其已进行了前降支的开通,有明确的影像学证据证明血运已重建。并随着患者心包压力的瞬间释放,压迫症状解除,其血流动力学状态逐渐恢复稳定。在辅助机器逐渐撤除后进行延迟关胸中,我们观察到,心肌水肿吸收速度是较为迅速的,5天时间即可恢复至相对正常大小,但其心功能并未能恢复至较为理想的范畴,主要考虑其存在广泛前壁心肌梗死的因素,其长期仍需进一步的随访以观察本次手术的远期效果。小结在介入临床工作中,发生心包填塞后仍需高度思考其病因,最好是在影像学基础上进行相关抢救性措施,尤其是B超的运用。切勿轻易进行有创操作,并需做好与外科系统的有效衔接。作好有效评估才是成功抢救的基础。
原始出处:
许万紫, 曹海龙, 王东进. 罕见介入术中非因冠脉破裂引发心包填塞经急诊抢救成功1例. 临床急诊杂志. 2018. 19(03): 204-206.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











非常有用.谢谢分享
55
#心包填塞#
39
#罕见#
41
#抢救#
47
好文献学习了
0
典型危重病例.学习了.
46