Mol Cell:程序性细胞坏死执法方式:MLKL引发细胞膜完整性破坏
2014-04-23 孙学军 科学博客
细胞死亡是维持多细胞生物组织结构稳态的重要手段,细胞死亡包括细胞凋亡和程序性坏死两种重要类型,两种细胞死亡类型的最关键区别是细胞膜完整性,细胞凋亡是保持细胞膜完整性的细胞萎缩,即使到最终的细胞片段形成仍保持细胞膜包绕,这种死亡方式的最大特点是能限制炎症反应的过度发生。而程序性坏死(Programmed necrotic cell death)的特征表现 是细胞膜完整性的破坏,导致细胞内物质释放
细胞死亡是维持多细胞生物组织结构稳态的重要手段,细胞死亡包括细胞凋亡和程序性坏死两种重要类型,两种细胞死亡类型的最关键区别是细胞膜完整性,细胞凋亡是保持细胞膜完整性的细胞萎缩,即使到最终的细胞片段形成仍保持细胞膜包绕,这种死亡方式的最大特点是能限制炎症反应的过度发生。而程序性坏死(Programmed necrotic cell death)的特征表现 是细胞膜完整性的破坏,导致细胞内物质释放,细胞内物质释放会引起明显的炎症反应。多细胞生物进化出两类细胞死亡方式各有重要意义,例如肿瘤的发生就是细 胞凋亡无法正常执行,导致细胞过度增生,所以许多肿瘤治疗方法是通过提高细胞凋亡实现。细胞坏死在发育、对抗病毒感染和引起组织损伤等方面也具有十分重要 作用。由于细胞坏死和炎症反应关系更密切,因此,最近10多年,许多生物学家对这一细胞死亡现象十分关注。国内北京的王晓东院士和厦门的韩家淮院士,美国哈佛大学医学院细胞生物学系终身教授,美国艺术和科学院院士袁均瑛都是这一领域的代表性人物。
在程序性坏死的信号传导机制研究方面,比较明确的是一种细胞死亡复合物,这种细胞死亡复合物关键的功能分子是两个蛋白激酶RIP1和RIP3传递死亡信号。其上游引起这些信号的启动信号包括肿瘤坏死因子受体家族Toll-like的受体家族。其下游分子是目前研究的热点领域。王晓东实验室在何苏丹博士2009年发现了RIP3是在细胞程序性坏死通路必不可少的信号传递蛋白后,过去几年努力攻克蛋白激酶如何引起细胞坏死的难题。该团队2012年率先发现了RIP3的特异性底物蛋白MLKL。发现MLKL是拥有激酶结构域但无激酶功能的假激酶,其激酶结构域375位苏氨酸和358位丝氨酸在细胞程序性坏死被启动时被RIP3磷酸化。MLKL磷酸化是细胞程序性坏死通路中不可或缺步骤 (Sun et al., Cell 148, 213)。厦门韩家淮实验室最近也针对MLKL在细胞程序性坏死作用方面开展研究。
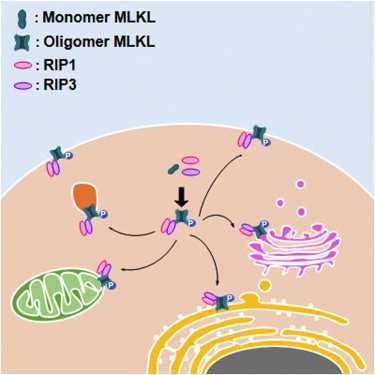
这次发表王晓东实验室发表的论文将目光关注在细胞程序性坏死细胞膜破坏这个特征现象和MLKL的关系上,这次研究他们首先证明了药物诱导的人类肝细胞损伤存在细胞程序性坏死的特征,并通过建立新的MLKL磷酸化抗体,确定了MLKL在引起细胞膜完整性破坏的分子过程,MLKL磷酸化会从单体形成寡聚体,并从细胞浆转移到细胞膜,这些MLKL寡聚体N末能插入细胞膜结构内与脂类物质磷脂酰肌醇和心磷脂结合,这种结合能使细胞膜完整性破坏形成孔道(间接证据),这种孔道导致细胞内物质的释放,研究中发现即使像右旋糖甘这样的大分子都可以释放,说明这种破坏十分严重,这种细胞膜破坏必然会产生细胞坏死的后果。

随着程序性细胞坏死分子机制研究的深入,这种研究模式将逐渐成为许多疾病研究的标准模式,在早期的这些学者,将为以后的大量研究提供关键研究方法,例如袁的 细胞坏死阻断剂和这次研究中的磷酸化抗体,都给许多研究提供了关键工具。感谢这些学者给这一领域的突出贡献,更喜见中国和华人学者在这一领域的关键作用。
原始出处:
Wang H, Sun L, Su L, Rizo J, Liu L, Wang LF, Wang FS, Wang X. Mixed Lineage Kinase Domain-like Protein MLKL Causes Necrotic Membrane Disruption upon Phosphorylation by RIP3.Mol Cell. 2014 Apr 10;54(1):133-46
相关文献:
Chen X, Li W, Ren J, Huang D, He WT, Song Y, Yang C, Li W, Zheng X, Chen P, Han J.Translocation of mixed lineage kinase domain-like protein to plasma membrane leads to necrotic cell death.Cell Res. 2014 Jan;24(1):105-21.
Chen W, Zhou Z, Li L, Zhong CQ, Zheng X, Wu X, Zhang Y, Ma H, Huang D, Li W, Xia Z, Han J.Diverse sequence determinants control human and mouse receptor interacting protein 3 (RIP3) and mixed lineage kinase domain-like (MLKL) interaction in necroptotic signaling.J Biol Chem. 2013 Jun 7;288(23):16247-61
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#MLKL#
33
#细胞膜#
32
#完整性#
26
#CEL#
24
#坏死#
24
#Cell#
22