Ann Oncol:贝伐珠单抗可显著提高卵巢癌患者生存率!
2017-05-08 tianxuexin MedSci原创
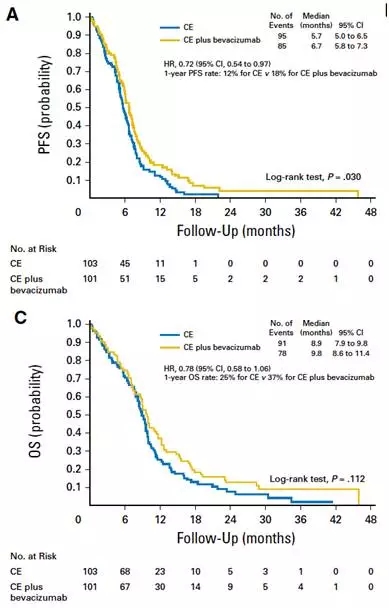
背景:在开放标签随机III期AURELIA试验中,将贝伐珠单抗联合铂化疗卵巢癌(PROC)的化学疗法相比单独使用化学疗法改善了无进展生存期和反应率,但没有提高总体生存率(OS)。该研究评估了贝伐珠单抗用于单独化疗后疾病进展(PD)的患者的疗效。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#患者生存#
0
#Oncol#
20
#贝伐珠#
37
#生存率#
0
#贝伐#
24
说说,小编是不是也收好处费啦?这种药品疗效与价格极其不和谐
87