病例:武侠中的“三尸虫”竟然真的存在
2018-04-28 成骢,魏洪霞,池云 MedSci原创
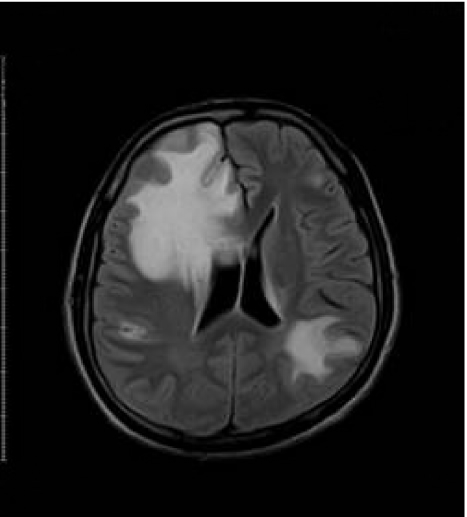
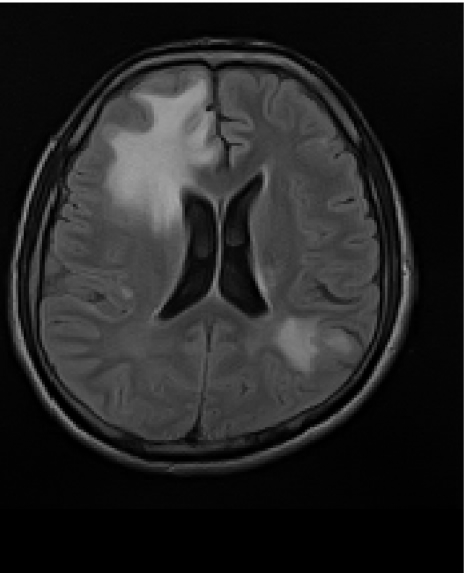
经典武侠小说《笑傲江湖》中,日月神教用阴损至极的“三尸脑神丹”控制教众,每年端阳节午时,若无解药,便会尸虫入脑,让人痛苦不已。而现实中有一种被称之为“三尸虫”的寄生虫,导致了本例患者的头痛、恶心、癫痫等。究竟是怎么一回事呢?

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习一下很不错
85
可以的
87
学习了很多先进的医学知识
72
学习谢谢分享!
102
很好.学习了
76
涨知识了
32
学习了谢谢分享!!
30
好知识值得拥有的
26