Nature:再生技术让盲鼠复明 为治疗视网膜色素变性等致盲疾病带来希望
2018-08-21 赵熙熙 中国科学报
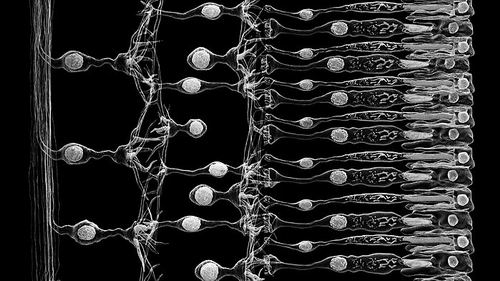
人眼中有一些细胞能够修复视力受损疾病造成的伤害。但到目前为止,科学家还没有成功地让它们发挥功效。如今,一个研究小组声称,他们已经促使这些细胞——被称为“米勒胶质细胞”——在老鼠的眼睛里再生了一种光受体细胞。根据科学家8月15日发表在英国《自然》杂志上的研究结果,这些新细胞可以探测到射入的光线,并与眼睛中的其他细胞结成网络向大脑传递信号,而这正是逆转某些遗传眼病和损伤的潜在步骤,这也为治疗视网膜色素
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
23
#色素#
33
#视网膜色素变性#
37
#视网膜#
33
#变性#
36