Sci Rep:恩杂鲁胺可以抑制睾丸素诱导的人类前列腺癌异种种植体的生长
2017-11-05 AlexYang MedSci原创
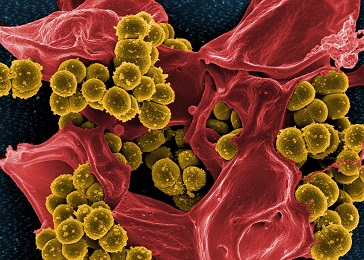
斑马鱼已经成为一种非常流行的人类肿瘤异种种植模型,尤其是对包括前列腺癌(PCa)在内的实体瘤。到目前为止,在斑马鱼中睾丸素存在情况下的异种种植体研究还没有进行过,甚至在雄激素依赖的细胞模型中,如LNCaP细胞系中,也没有进行过类似的研究。最近,有研究人员为了探究PCa在人类激素环境中发展的建模,他们研究并确定了外源睾丸素对LNCaP生长的影响,或者在斑马鱼胚胎中雄激素依赖的C4-2细胞异种种植情况
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#种植#
24
#种植体#
28
#睾丸#
29
#睾丸素#
37
好好好好好学习学习学习
57