AGING CELL:长寿基因可稳定衰老转录组,并应对内部应激
2019-02-18 海北 MedSci原创
至今为止,我们关于衰老过程中转录组变化的作用和调节机制尚不清楚。研究人员已经提出,由于转录因子与年龄相关的下调,转录组在衰老期间遭受衰退。
至今为止,我们关于衰老过程中转录组变化的作用和调节机制尚不清楚。研究人员已经提出,由于转录因子与年龄相关的下调,转录组在衰老期间遭受衰退。
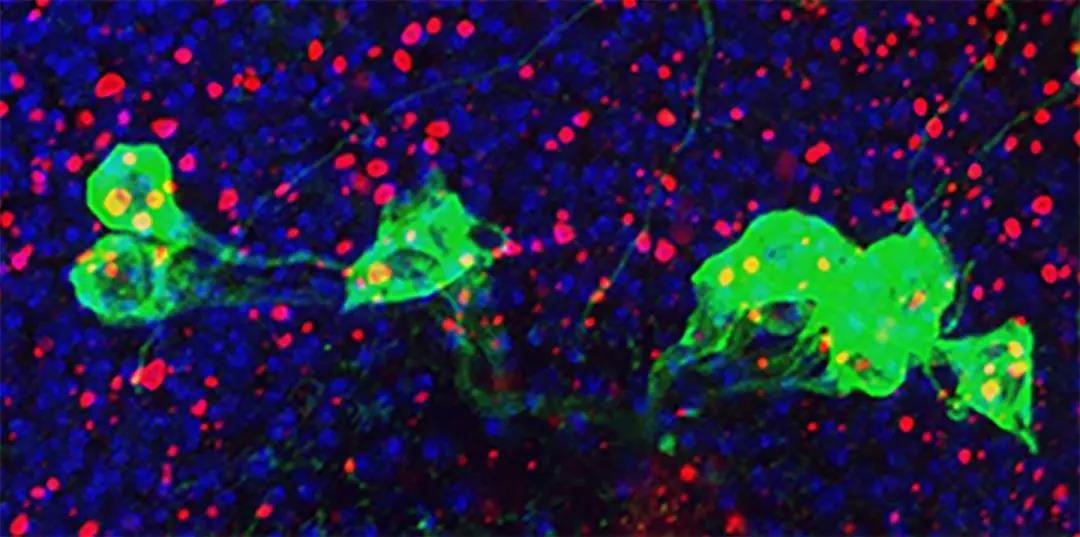
在最近的一项研究中,研究人员描述了转录因子DAF-16的作用。在秀丽隐杆线虫的正常衰老过程中,DAF-16是一种高度保守的寿命调节剂。研究人员发现,DAF-16可以易位到老年野生型线虫的细胞核中,并激活数百个基因的表达,以响应与年龄相关的细胞应激。大多数年龄依赖性DAF-16靶标与胰岛素信号传导下游的经典DAF-16靶标不同。
该证据和其他证据表明,DAF-16在衰老过程中的激活不同于DAF-16的经典激活,因为DAF-2的信号传导减少。进一步的分析表明,这部分是由于衰老过程中蛋白质稳态的丧失引起的。
研究人员还发现,如果没有daf-16,早在成虫第2天就会发生显着的基因表达变化,这表明DAF-16在正常衰老期间起稳定转录组的作用。
因此,该研究结果表明,正常衰老不仅仅是一个基因表达程序由于失去监管活动而陷入混乱的过程;相反,在衰老过程中存在活跃的转录调节。
原始出处:
Shang‐Tong Li et al. DAF‐16 stabilizes the aging transcriptome and is activated in mid‐aged Caenorhabditis elegans to cope with internal stress. Aging Cell, 2019; doi: https://doi.org/10.1111/acel.12896
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#转录#
41
#CEL#
0
#Cell#
31
#转录组#
32
#应激#
34
#长寿基因#
54