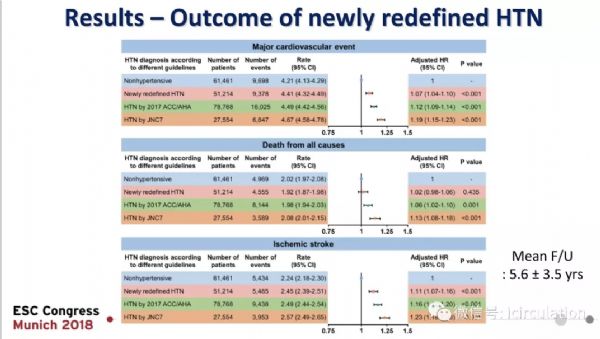
Hypertension:高血压诊断标准若降至130/80mmHg,高血压患病率会大幅大增加
2018-09-04 MedSci MedSci原创
Julio A.Lamprea-Montealegre等人尝试根据用于诊断的血压(BP)阈值评估美国人高血压的患病率和高血压成人患者的特征,并评估其相关心血管疾病风险。本研究纳入2013-2014年国家健康与营养调查研究中的5389位年满20岁的成年人,并招募了SPRINT(收缩压干预试验)的9361位受试者和ACCORD-BR试验(运动控制糖尿病-血压心血管风险)的4733位受试者。在国家健康与
本研究纳入2013-2014年国家健康与营养调查研究中的5389位年满20岁的成年人,并招募了SPRINT(收缩压干预试验)的9361位受试者和ACCORD-BR试验(运动控制糖尿病-血压心血管风险)的4733位受试者。
在国家健康与营养调查研究中,患病率为在两个不同场合观察到血压升高的概率。采用新的高BP阈值: ≥130/80 mmHg,约新增2400万美国成年人会被诊断为高血压,430万人会被推荐开始服用抗高血压药物。该人群平均动脉粥样硬化性心血管疾病风险和心血管疾病患病率均要低于SPRINT和ACCOD-BP的受试者(17% vs 22%和27%;9% vs 17%和34%)。在SPRINT和ACCOD-BP中,仅小部分(9%和13%)个体在初始时未采用抗高血压药物治疗,这些个体患心血管疾病的发生率明显低于基础即采用降血压药物治疗的个体。
综上所述,采用美国心脏病学院/美国心脏协会指南会导致美国成人高血压患病率和推荐进行降血压治疗的成人数量大幅度增加。这些人的心血管风险因素明显低于既往两个大型BP试验中的大多数个体。
Julio A.Lamprea-Montealegre,et al. Prevalence of Hypertension and Cardiovascular Risk According to Blood Pressure Thresholds Used for Diagnosis. Hypertension.8 Aug 2018. 2018;72:602-609
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#TENS#
34
#高血压患病率#
38
#PE#
32
^_^^_^^_^^_^
61
#患病率#
32
#诊断标准#
30
#Hypertension#
28
不错的文章值得拥有
68