ANN RHEUM DIS:B细胞OX40L支持滤泡辅助性T细胞发育并导致SLE发病
2017-08-18 xiangting MedSci原创
两种模型全身自身免疫病理改善表明OX40L是SLE治疗中的优良靶点。
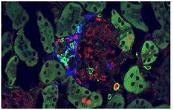
TNFSF4(编码OX40L)是系统性红斑狼疮(SLE)的易感基因。风险等位基因增加细胞系中TNFSF4的表达,但是将这种作用与疾病联系起来的机制尚不清楚,介导这种风险的OX40L表达细胞类型尚不明确。已经证明阻断OX40L可以在几种自身免疫模型中降低疾病严重程度,但不包括SLE。这项研究旨在探讨其在狼疮中的潜在治疗作用。
使用条件敲除小鼠系来研究B和T淋巴细胞上的OX40L在全身自身免疫中的功能。
生理上,B和T细胞上的OX40L都引起体液免疫应答,但B细胞OX40L支持继发性体液应答和抗体亲和力成熟。数据还表明,B细胞OX40L的缺失阻碍了脾滤泡辅助性T细胞的产生。在两种SLE模型中,自发同类模型和H2-IA bm12移植物抗宿主诱导模型,B细胞OX40L缺失改善自身免疫表型。在每种情况下,这种改善伴随着滤泡辅助性T细胞数量的减少。重要的是,在这些模型中种系敲除并不表现出与B细胞敲除明显不同的表型。
这些发现可以建立一种基因决定的增加OX40L表达通过几种机制促进人类SLE发病的模型,这取决于其细胞表达。两种模型全身自身免疫病理改善表明OX40L是SLE治疗中的优良靶点。
原始出处:
Andrea Cortini, et al. B cell OX40L supports T follicular helper cell development and contributes to SLE pathogenesis. ANN RHEUM DIS. 17 August 2017.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Dis#
28
#OX40#
32
#辅助性T细胞#
44
#B细胞#
29
#SLE#
27
#发育#
18
很好,不错,以后会多学习
41
学习了,好文章
38