本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2018-04-04 王传彬 方梦诗 韦超 功能与分子医学影像学杂志(电子版)
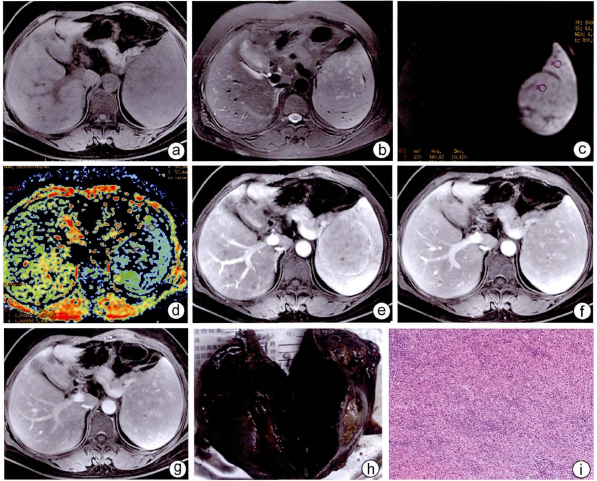
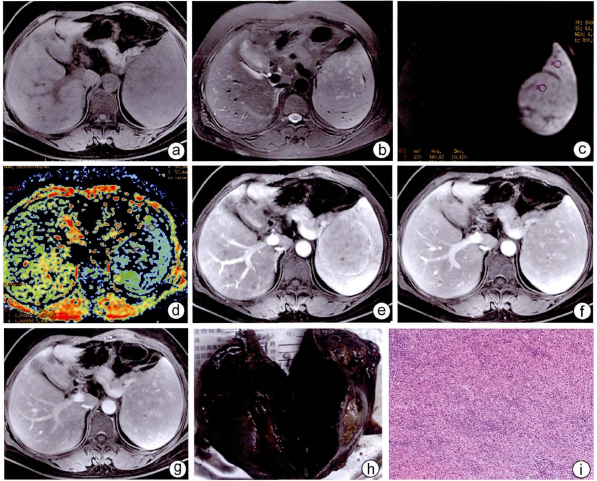
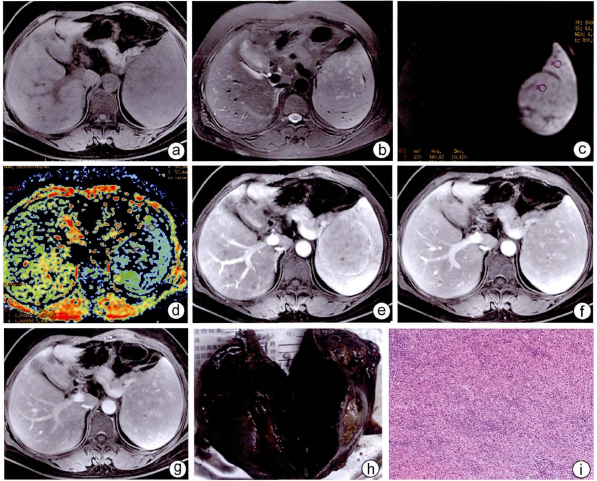
患者女,47岁,左侧腰部酸痛不适3个月以上。

阿尔兹海默症(俗称老年性痴呆症)常常被认为是一种与年龄相关的、发生在老年阶段的疾病。然而,生命科学学院张研课题组通过实验证明在家族型阿尔兹海默症小鼠模型中,神经元发育、蛋白运输、轴突起始节功能等方面在发育的早期就表现出了显著的缺陷。Ankyrin G (AnkG)是一种重要的锚定蛋白,对于轴突起始节处的过滤筛选功能起着至关重要的作用。张研课题组的研究发现,在早期阿尔兹海默症模型小鼠中,mi
三阴性乳腺癌在全球乳腺癌患病女性中占15~20%,这种乳腺癌亚型具有复发早,复发率高的特点,因此患有三阴性乳腺癌的病人生存几率很低,这也与缺少靶向治疗策略具有很大关系。找到三阴性乳腺癌的生物学标记对于三阴性乳腺癌早期诊断及制定有效的治疗方法具有非常重大的意义,同时也是当务之急。
本期为大家介绍一篇基于观察研究的系统回顾来评估miR-148/miR-152家族在癌症患者中预后价值的文章。文章发表在Oncotarget期刊上,题目为Evaluatingthe prognostic value of miR-148/152 family in cancers: based on a systemicreview of observational studies(基于观察研究的系
来自德克萨斯MD安德森癌症中心的研究人员发现,一个叫做miR-200的microRNAs家族可通过抑制肿瘤编织新的血管支持自身的能力,阻断肿瘤的发展和转移。研究报告发表在9月10日的《自然通讯》(Nature Communications)杂志上。【原文阅读】 研究人员发现,如果肺癌、卵巢癌、肾癌或三阴性乳腺癌患者体内表达高水平的miR-200,这些患者寿命会更长一些。 随后


梅斯医学MedSci APP
医路相伴,成就大医
谢谢分享学习
32
#错构瘤#
52
学习了.谢谢分享
41
好好学习天天向上
40