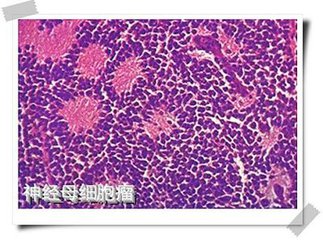
JCO:切除程度对COG A3973研究中高风险神经母细胞瘤患者的局部控制和生存率的影响
2016-11-25 MedSci MedSci原创
这项分析评价了COG A3973研究中原发性肿瘤切除程度对于患者局部进展和生存率的影响,同时评价临床与成像检查预估切除程度的一致性。
这项分析评价了COG A3973研究中原发性肿瘤切除程度对于患者局部进展和生存率的影响,同时评价临床与成像检查预估切除程度的一致性。
分析队列共入组220例进行原发部位肿瘤切除术并复查的患者。切除程度<90%或≥90%的患者均可入组,关于切除程度的数据源自手术医师的评估(所有患者)。其中84名患者的切除程度采用计算机断层扫描成像检查,并比较评价结果一致性。治疗结果包括无事件存活(EFS),总生存(OS)和局部进展的累积发生(CILP)。
外科医生评估的切除程度在154例(70%)患者中为≥90%,在66例(30%)患者中为<90%。所有入组患者的5年EFS,OS和CILP(±SE)分别为43.5%±3.7%,54.9%±3.7%和11.9%±2.2%。其中,≥90%患者组的EFS(45.9%±4.3%)高于<90%患者组(37.9%±7.2%; P = 0.04),而CILP则相反。(≥90%患者组:<90%患者组=8.5%±2.3%:19.8%±5.0%,P = 0.01)。在多变量分析中可看出,在调整MYCN扩增或二倍体后,≥90%患者组的EFS会相应延长,但OS无显著影响。医生经验评估切除程度与系统成像评估程度一致性较低,仅达到63%。
尽管临床医生评估与系统成像评估程度存在不一致性,但是外科评估切除程度≥90%的患者组获得了更好的EFS和更低的CILP。但延长OS在这类疾病中仍是一种挑战。这一结果表明,针对高复发风险神经母细胞瘤患者,其切除程度≥90%对于患者有较好的生存获益。
原文出处: Allmen Dv, Davidoff AM, London WB, Ryn CV, Haas-Kogan DA, Kreissman SG, et al. Impact of Extent of Resection on Local Control and Survival in Patients From the COG A3973 Study With High-Risk Neuroblastoma. Journal of Clinical Oncology;0:JCO.2016.67.642.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#母细胞瘤#
35
#JCO#
23
#高风险#
29
#973#
32
不错
62
值得参考、借鉴
60
学习了,分享了。
59
#生存率#
21
#局部#
23
#细胞瘤#
27