Nat Med:“饿死”癌细胞为何总失败?Science子刊已破解谜题
2018-01-30 佚名 生物探索
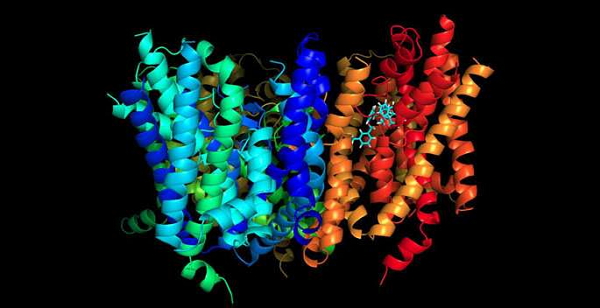
新年伊始,“饿死癌细胞”领域成果频出!不久前,一篇Nature Medicine论文首次证实,一种新型化合物能够切断肿瘤氨基酸代谢通路,从而抑制肿瘤生长。而本月发表在Science子刊上的一项研究则首次揭示了为什么癌细胞不容易被“饿死”,并提出了一种新型疗法。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
29
#癌细胞#
30
#SCIE#
28
#Med#
33
学习
49
学习了新知识
63