NEJM:胃穿孔导致气腹-病例报道
2019-07-04 xing.T MedSci原创
探查性腹腔镜检查显示胃后壁有穿孔,没有腹腔液或其他小肠或大肠异常。认为胃破裂是由复苏期间急性胃扩张气压伤引起的。患者进行了穿孔手术修复。
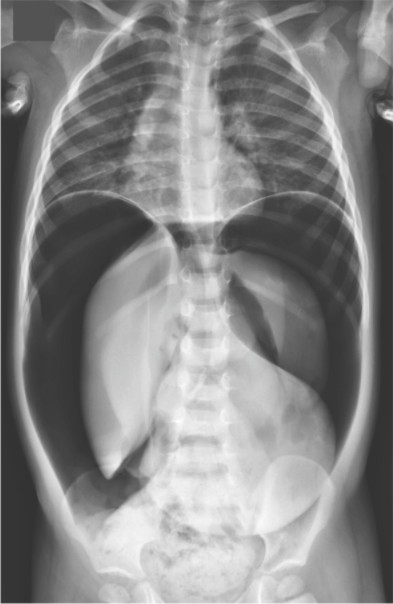
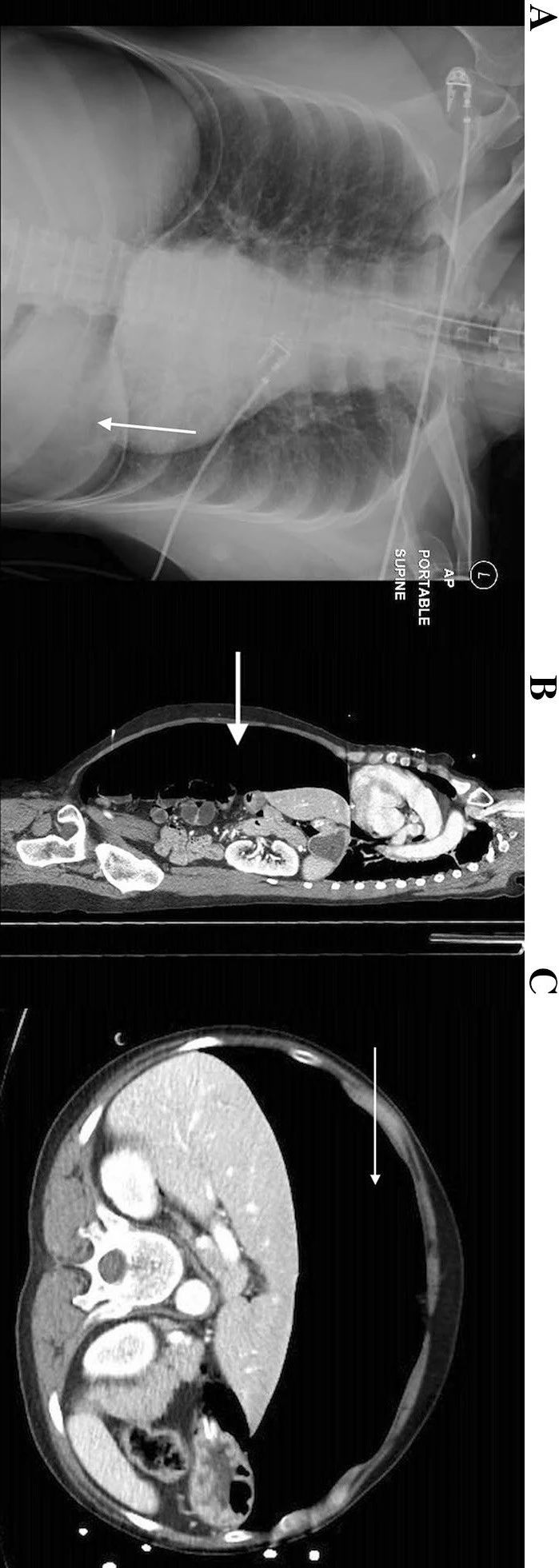
患者为一名两岁半的男孩,在发热性上呼吸道疾病期间出现癫痫发作后被送往急诊就诊。目睹癫痫发作的成年人担心这名男孩已经呼吸停止并开始进行胸部按压和人工呼吸。大约1分钟后,男孩恢复知觉。
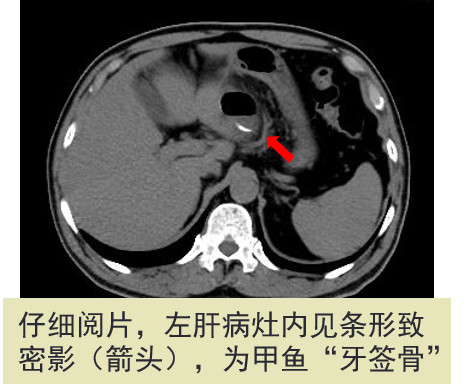
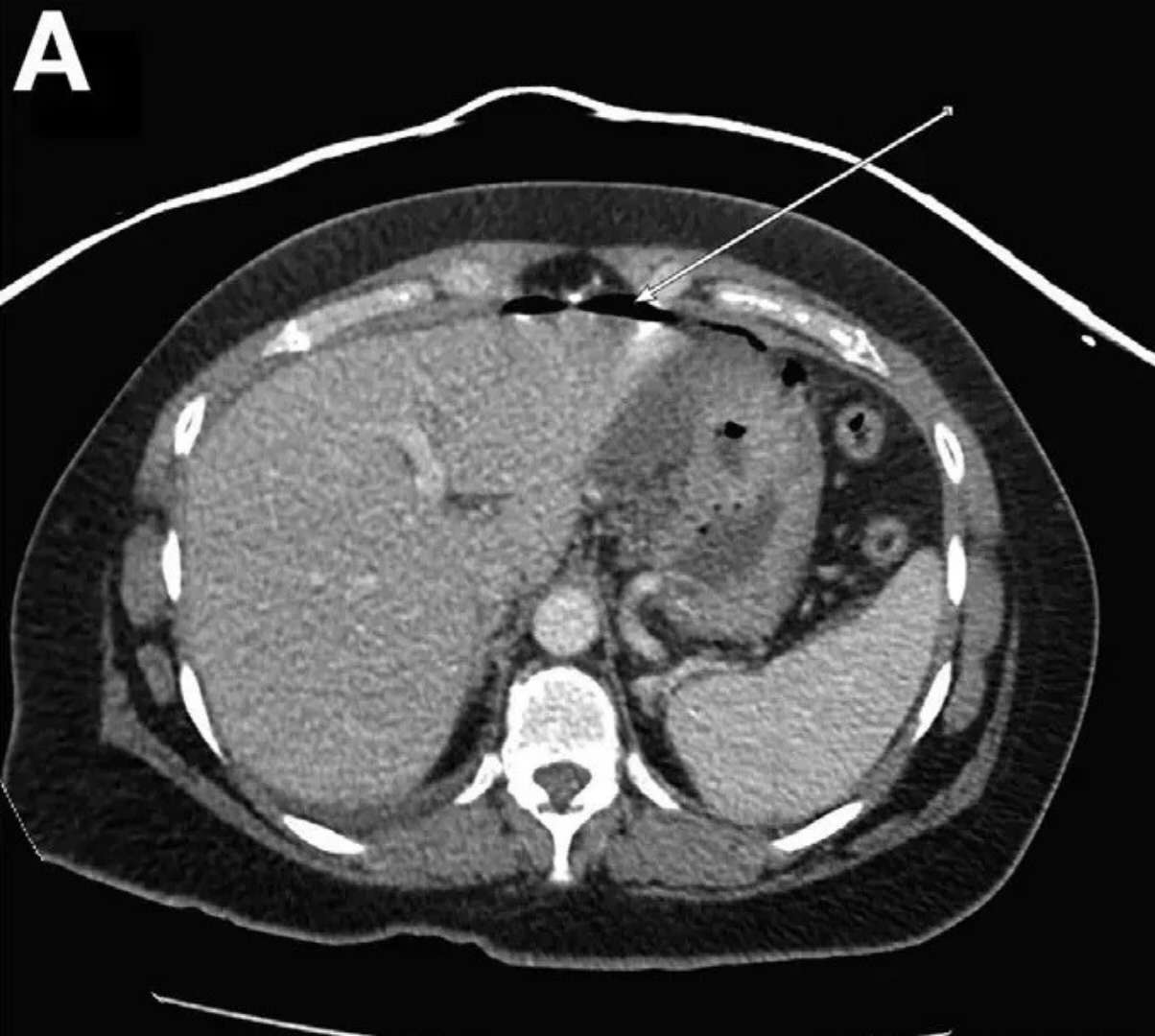
在体格检查中,他神志清醒,神经系统检查显示没有异常。他看起来很不舒服,腹部肿胀,呈鼓状,压痛。腹部射线照相显示气腹。没有发现肋骨骨折。探查性腹腔镜检查显示胃后壁有穿孔,没有腹腔液或其他小肠或大肠异常。认为胃破裂是由复苏期间急性胃扩张气压伤引起的。患者进行了穿孔手术修复。
患者在医院住了3天,没有观察到额外的胃肠道问题或癫痫发作。他从手术和上呼吸道疾病中恢复得很顺利。
在6个月后的一次随访中,他正常成长并发育良好。
原始出处:
Alexandra Masson,et al.Pneumoperitoneum from a Gastric Perforation.N Engl J Med 2019;https://www.nejm.org/doi/full/10.1056/NEJMicm1814352
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#气腹#
33
#穿孔#
47
#胃穿孔#
46
这样就可以发新英格兰?
72
mark
71
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
52