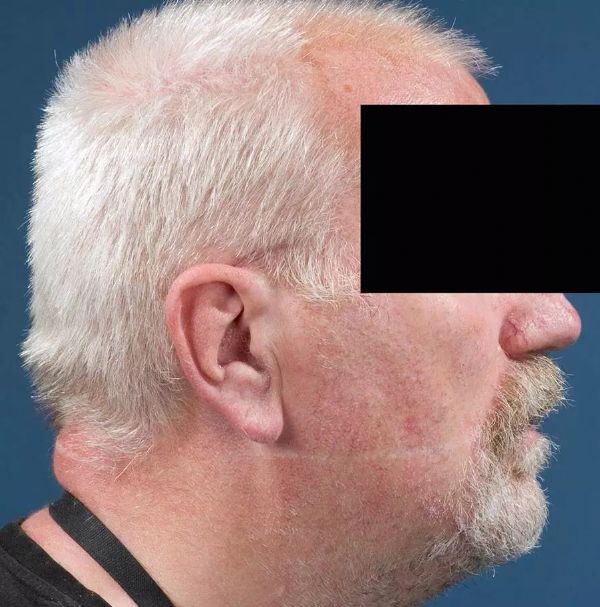
Intensive Care Med:气管插管固定绳引起面部瘢痕一例
2017-10-11 重症行者翻译组 重症医学
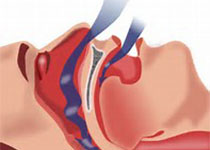
对于接受机械通气的ICU患者来说,气管内插管(endotracheal tube,ETT)的固定是必不可少的。固定失效可引起ETT滑脱、气道损伤、脱位或意外拔管。常用的固定方法有:棉绳、胶布或商用的气管插管固定器。若固定ETT时对面部产生的压力过大,则可导致面部皮肤和粘膜产生永久性的损伤。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TENS#
23
#瘢痕#
26
#气管插管#
30
#Med#
20
大千世界.无奇不有.从来没见过这样的
48