Saudi Med J:非典型后巩膜炎类似的脉络膜黑色素瘤病例报告
2018-05-15 cuiguizong MedSci原创
沙特国王大学医学院眼科学系的Alsharif HM近日在Saudi Med J发表了一项病例,他们报告一例非典型后巩膜炎与无色素脉络膜黑色素瘤相似。
沙特国王大学医学院眼科学系的Alsharif HM近日在Saudi Med J发表了一项病例,他们报告一例非典型后巩膜炎与无色素脉络膜黑色素瘤相似。
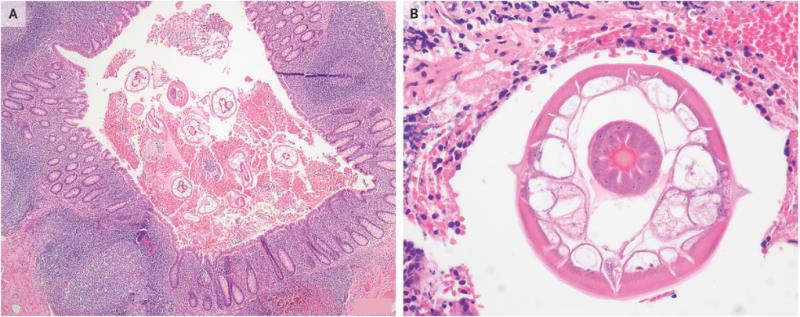
这是一名30岁的健康菲律宾男子,在左眼没有疼痛的情况下发生急性视力丧失。5个月左右后,被转诊到研究者的诊所中进行进一步的检查和治疗。检查时,左眼视力为20/200。前节检查结果不明显,伴有结膜静脉和巩膜外静脉充血,而眼底检查显示具有非色素性脉络膜肿块,伴有明显的视网膜下充液,类似于无黑色素脉络膜黑色素瘤。右眼检查结果并不明显。

该患者被诊断为非典型后巩膜炎,进行口服类固醇药物治疗2周后并没有明显改善。然后将类固醇药物注射到左眼眼周附件,结果发现脉络膜肿块大小急剧减少,视网膜下液体完全消除。注射药物治疗一个月后视力提高至20 / 28.5。
因此,他们认为及时治疗对于尽量减少视力威胁及其并发症至关重要。
原文出处:
Alsharif, H.M. and S.A. Al-Dahmash, Atypical posterior scleritis mimicking choroidal melanoma. Saudi Med J, 2018. 39(5): p. 514-518.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#巩膜炎#
42
#色素#
23
#脉络膜#
29
#脉络膜黑色素瘤#
42
#病例报告#
25
#非典型#
32
#黑色素#
28
#黑色素#
32
#Med#
32
学习学习学习
46