J Thorac Cardiovasc Surg:IA期肺腺癌肺段切除与肺叶切除疗效相似
2013-11-07 萧弈 dxy
对于肺叶切除和肺段切除临床IA期肺腺癌的肿瘤学结果是目前胸外科医生争论的焦点,但这方面数据仍比较缺乏。针对这种情况,来自日本广岛大学肿瘤外科的Morihito Okada教授等人进行了一项研究,研究结果在线发表于2013年8月23日的《心胸外科杂志》(J Thorac Cardiovasc Surg)杂志上。作者发现肺段切除适合于临床IA期肺腺癌,与那些标准肺叶切除术患者生存相似。【原文下载】该研
对于肺叶切除和肺段切除临床IA期肺腺癌的肿瘤学结果是目前胸外科医生争论的焦点,但这方面数据仍比较缺乏。针对这种情况,来自日本广岛大学肿瘤外科的Morihito Okada教授等人进行了一项研究,研究结果在线发表于2013年8月23日的《心胸外科杂志》(J Thorac Cardiovasc Surg)杂志上。作者发现肺段切除适合于临床IA期肺腺癌,与那些标准肺叶切除术患者生存相似。【原文下载】
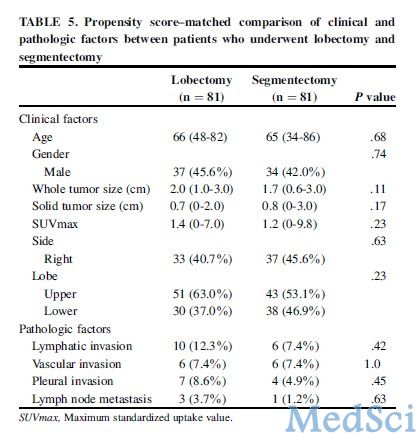
该研究回顾性分析618例中481例连续临床IA期肺腺癌患者,术前行高分辨率计算机断层扫描和F-18-脱氧正电子发射断层扫描/计算层析成像后接受肺叶切除或肺段切除。排除137例行楔形切除术患者。对所有行肺叶切除(n=383)和肺段切除(n=98)的患者及其手术结果进行了倾向分数匹配分析
研究结果表明,无复发生存(RFS)和总生存(OS)在肺叶切除(3年RFS,87.3%;3年OS,94.1%)和肺段切除(3年RFS,91.4%;风险比[HR]0.57;95%可信区间[CI]0.27-1.20;P=0.14;3年OS,96.9%;HR=0.49;95%CI,0.17-1.38;P=0.18)患者之间未见明显差异。临床因素这两个治疗组之间存在显著差异如实体肿瘤大小(P<.001),最大标准摄取值(SUVmax)(P<.001),和肿瘤位置(左右侧,P=0.005;肺叶,P=0.001)。81例配对倾向分数匹配分析发现变量包括如年龄、性别、实体肿瘤大小、SUVmax、左右侧和肺叶,RFS和OS在肺叶切除(3年RFS,92.9%;3年OS,93.2%)和肺段切除(3年RFS,90.9%;3年OS,95.7%)之间相似。
该研究发现,肺段切除适合于临床IA期肺腺癌,与那些标准肺叶切除术患者生存相似。
原文出处
Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M, Okada M.Oncologic outcomes of segmentectomy compared with lobectomy for clinical stage IA lung adenocarcinoma: propensity score-matched analysis in a multicenter study.J Thorac Cardiovasc Surg. 2013 Aug;【原文下载】
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#THORAC#
27
#ASC#
20
#肺叶切除#
35