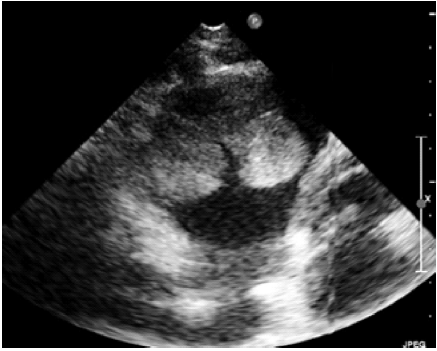
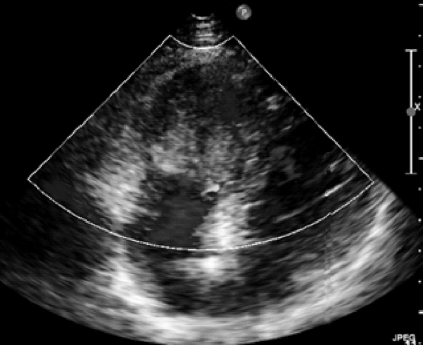
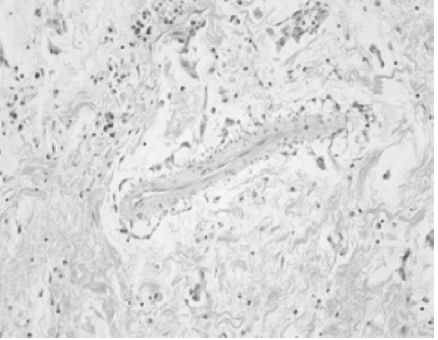
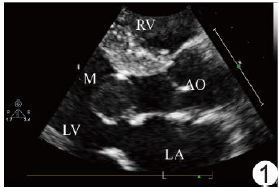
超声心动图诊断右心室黏液瘤1例
2019-03-17 杨德顺 卢华红 朱佳 心脑血管病防治
患者,女性,28岁,因“反复心慌1年余”住院。查体:体温36.7℃,心率82次/分,呼吸19次/分,血压111/80mmHg,锁骨上淋巴结未及肿大,两肺呼吸音清,心律齐,未闻及病理性杂音,未及心包摩擦音,双下肢未见浮肿。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#心动图#
28
#黏液瘤#
27
#右心室#
32
学习了,谢谢分享!
65