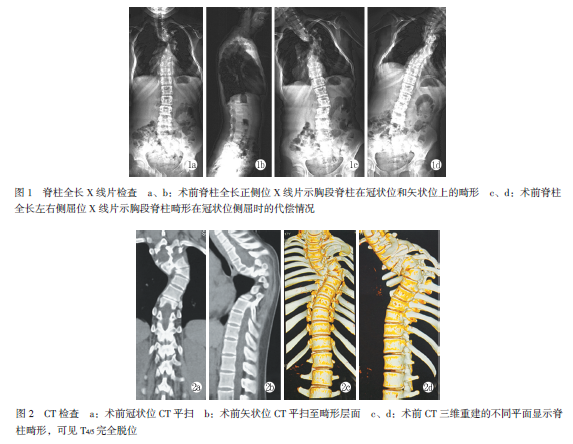
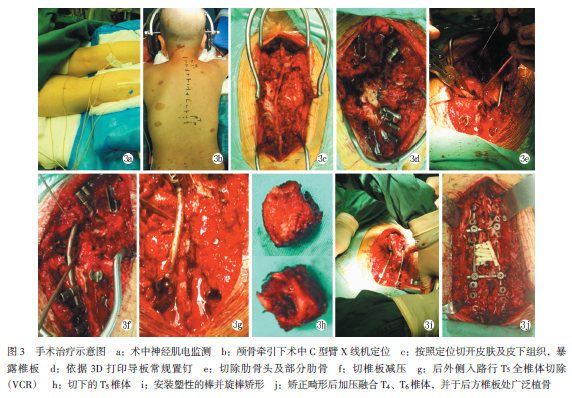
I型神经纤维瘤病脊柱侧后凸并椎体完全脱位:1例
2019-06-12 潘俊杰 王兵 陈钰琳 中国矫形外科杂志
患者,女,17岁。出生时正常,儿童时期生长发育落后于同龄儿童,6岁时因发现脊柱畸形伴全身多发咖啡样斑点至医院就诊,行相关检查和基因筛查,具体结果及治疗不详,随后未引起重视。近十年来脊柱畸形逐渐加重并影响生活质量,但均未出现相应脊髓及神经损伤情况。入院前10d左右,患者晨起时感觉下肢无力及麻木,随后症状逐渐加重送至本院神经内科就诊,转诊前的2周内,患者下肢无力及麻木情况进行性加重。患者家族中无类似病

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#椎体#
36
#纤维瘤#
34
#神经纤维#
34
#脱位#
38
#纤维瘤病#
42