ANN ONCOL:选择性RET酶抑制治疗RET改变肿瘤患者
2018-08-28 MedSci MedSci原创
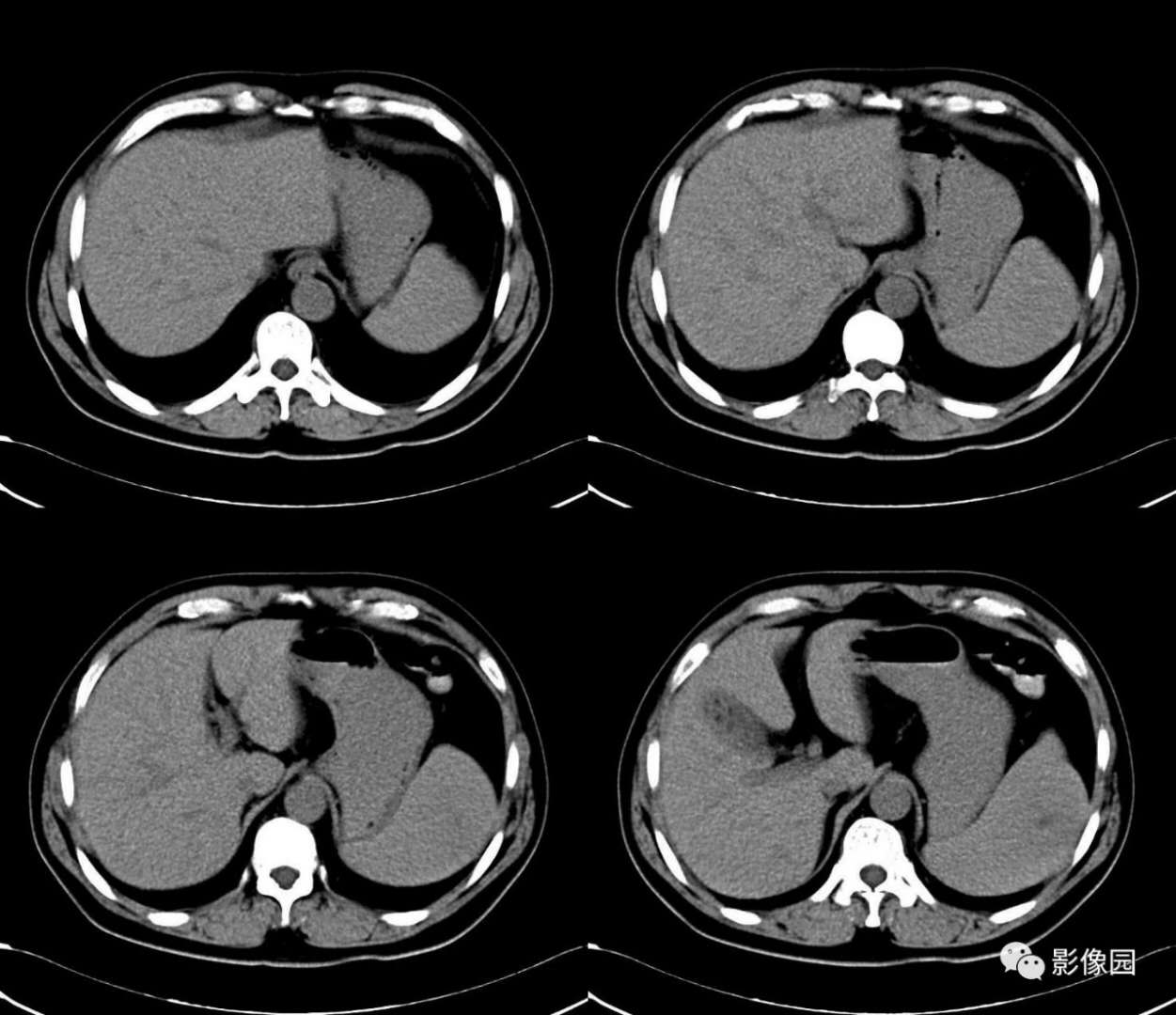
肺癌、甲状腺癌及其他肿瘤中RET酶相关改变对肿瘤发病具有意义。但是,具有抗RET活性的多酶抑制剂(MKI)治疗RET患者的临床抗肿瘤活性有限,使得靶向RET疗法的潜力受到质疑。LOXO-292是一种选择性RET抑制剂,可以抑制活化突变和获得性耐压突变。ANN ONCOL近期发表了一篇文章,研究其治疗RET改变肿瘤的有效性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#RET#
22
#选择性#
30
#Oncol#
0
#肿瘤患者#
34
不错的文章值得拥有哦
65