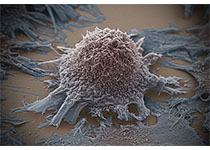
Nat Immunol:研究发现影响肺癌患者存活时间的重要因素!
2017-06-20 枫丹白露 来宝网
近年来,免疫治疗是一种新兴的攻击肿瘤细胞的癌症治疗技术,吸引了大众的想象力。当它发挥作用时,结果是惊人的。但是,通常情况下,科学家们仍然不知道为什么这样作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
31
#肺癌患者#
24
#研究发现#
27
#存活时间#
37
多研究,多发现,全面提高疗效!
59
学习了
54
学习了,谢谢作者分享!
51