ASCO-GU 2018:转移性生殖细胞肿瘤的诊断和治疗进展
2018-02-13 作者 | 纪长威 郭宏骞(南京大学医学院附属鼓楼医院) 编辑 | 豆豆(中国医学论坛报) 中国医学论坛报今日肿瘤
ASCO GU虽然名为泌尿生殖肿瘤研讨会,但从其日程来看,泌尿肿瘤占据了绝对支配地位。为期三天的会议共分为九大节段,其中前列腺癌独占三节,肾癌和膀胱癌各占两节,肾上腺肿瘤一节,生殖细胞肿瘤仅在一节中出现。我们将简要梳理关于睾丸肿瘤转移灶诊断和治疗的最新信息。
当地时间2月8~10日,2018年美国临床肿瘤学会泌尿肿瘤研讨会(ASCO GU)将于美国旧金山召开。本次会议的主题是“将科研证据转化为多学科照护(Translating Evidence to Multidisciplinary Care)”。
ASCO GU虽然名为泌尿生殖肿瘤研讨会,但从其日程来看,泌尿肿瘤占据了绝对支配地位。为期三天的会议共分为九大节段,其中前列腺癌独占三节,肾癌和膀胱癌各占两节,肾上腺肿瘤一节,生殖细胞肿瘤仅在一节中出现。我们将简要梳理关于睾丸肿瘤转移灶诊断和治疗的最新信息。
由于睾丸肿瘤原发灶的手术相对简单,涉及睾丸肿瘤的5个汇报均为其转移灶的监测和治疗。来自印第安纳大学的Mark Tann教授首先汇报了生殖细胞肿瘤化疗后腹膜后病灶的影像学监测,他指出,从经济、时效性和可操作性来讲,增强CT仍然是第一选择,MRI和PET/CT与增强CT有着相似的检出率。PET/CT对精原细胞瘤的阴性预测值(NPV)较高,阳性预测值(PPV)较低;而对非精原细胞瘤转移灶的检测价值有限。睾丸肿瘤手术及化疗后约66%的患者会检出腹膜后包块,但其中真正为有活性的转移灶占比很低。以精原细胞瘤为例,当腹膜后包块大于3 cm时,其中40%为有活性的转移灶;当包块小于3 cm时,仅有约8%为活性转移灶。由于睾丸癌腹膜后淋巴结清扫手术创伤性较大,因此术前判断腹膜后包块的性质至关重要。
来自荷兰肿瘤研究所的Joost Marijn Blok医生报道了他们对临床一期的睾丸癌腹膜后前哨淋巴结活检的经验。在阻断精索静脉后,向睾丸内注射放射性核素行SPECT/CT淋巴显像。根据淋巴显像结果进行腹腔镜前哨淋巴结切除活检和睾丸切除(图1)。然而,在淋巴显像阳性的23例生殖细胞肿瘤患者中,活检结果显示仅有3例(13%)为转移灶。此3例患者接受化疗,其余20例患者定期复查。中位随访期为63.9个月,无一例患者出现肿瘤复发(图2)。这也提醒我们,对睾丸肿瘤腹膜后淋巴结清扫手术的指征需严格掌握,避免过度治疗。前哨淋巴结活检在手术决策中有一定意义。
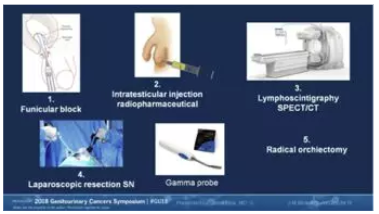
图1

图2
来自英属哥伦比亚大学的Christian Kollmannsberger教授进一步就避免过度治疗提供了证据。他的报道是关于肿瘤标志物阴性的临床二期睾丸癌的处理。研究表明相当比例的腹膜后淋巴结肿大为假阳性病灶,在随访中会逐渐缩小。即便证实为阳性病灶,其治疗效果也相当乐观,包括腹膜后淋巴结清扫手术、化疗、放疗等治疗后长期无复发生存(RFS)率都在90%以上(图3)。
Kollmannsberger教授的报告同时指出miRNA-371与睾丸癌腹膜后转移灶呈明显的正相关性,有望作为鉴别腹膜后包块良恶性的重要标志物。无独有偶,加拿大Princess Margaret Cancer Center的Ricardo Leao教授也在研究中证实miRNA-371a-3p对非精原细胞瘤腹膜后转移灶的准确预测作用(图4)。来自斯洛伐克考门斯基大学的Chovanec教授团队则强调了放疗和化疗对睾丸癌患者的远期毒副作用,尤其在性功能方面。他们对生存期超过5年的生殖细胞肿瘤患者进行了中位随访时间长达10年的随访,证实有10%~33%的幸存者存在严重的性功能障碍。
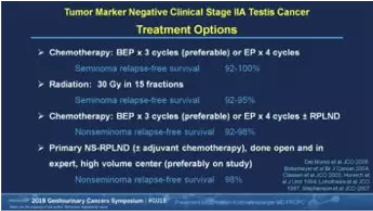
图3
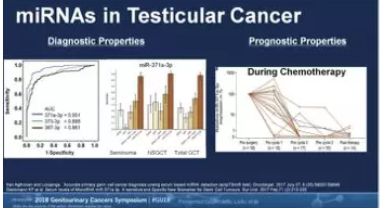
图4
上述报告使得原本对生殖细胞肿瘤“谈虎色变”的我们重新审视了其发生发展的过程,对手术、放疗或化疗等治疗决策的制定应该更加审慎。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#ASC#
47
#转移性#
38
#生殖细胞#
35
#生殖细胞肿瘤#
40