Circulation:在缺失CETP的情况下,ADCY9失活可抵抗动脉粥样硬化
2018-10-24 MedSci MedSci原创
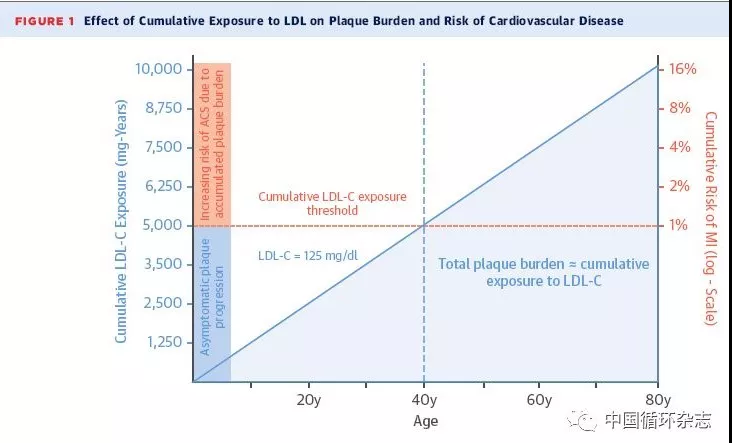
药物基因组学研究表明ADCY9基因型决定了CETP(胆甾醇酯转移蛋白)抑制剂达塞曲匹对心血管事件和动脉粥样硬化成像的影响。ADCY9和CETP活性相互作用的潜在机制尚未明确。研究人员采用进行或不进行CETP基因改造(CETPtgAdcy9Gt/Gt和CETPtgAdcy9WT)的Adcy9失活型(Adcy9Gt/Gt)和野生型(WT)小鼠进行动脉粥样硬化试验,予以注射表达功能获得性突变PCSK9(
研究人员采用进行或不进行CETP基因改造(CETPtgAdcy9Gt/Gt和CETPtgAdcy9WT)的Adcy9失活型(Adcy9Gt/Gt)和野生型(WT)小鼠进行动脉粥样硬化试验,予以注射表达功能获得性突变PCSK9(9型枯草杆菌蛋白酶/Kexin样前蛋白转化酶)的AAV8(腺相关病毒血清型8),并予以0.75%胆固醇饮食喂养16周。
与WT小鼠相比,Adcy9Gt/Gt小鼠动脉粥样硬化减少65%(p<0.01),斑块中CD68阳性巨噬细胞聚集和增殖也均减少(p<0.05),而且股动脉内皮依赖性血管舒张提高(p<0.01)。选择性药物阻断显示,NO、环氧化酶和内皮依赖性超极化通路均可促进Adcy9Gt/Gt小鼠血管舒张(p<0.01)。Adcy9Gt/Gt小鼠的动脉内皮细胞,相比WT小鼠的,可显著降低脾细胞的粘附性(p<0.05)。Adcy9Gt/Gt小鼠体重增加比胆固醇饮食的WT增加的多;这一点与全身脂肪组织量增加有关(p<0.01)。与WT小鼠相比,Adcy9Gt/Gt小鼠的喂养效率提高(P<0.01),同时心脏RR间隔延长(P<0.05),夜间心率变异性增加(p=0.0572)。在CETPtgAdcy9Gt/Gt小鼠中,Adcy9失活所诱导的对动脉粥样硬化、内皮功能、体重增加、脂肪组织体积和饲料效率的影响均消失(p>0.05)。
Adcy9失活可抵抗动脉粥样硬化,但只发生在CETP活性缺失的情况下。该抗动脉粥样硬化效应可能是由于动脉壁中巨噬细胞聚集、增殖减少以及内皮功能和自主张力增强所导致的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#粥样硬化#
26
#CETP#
35
#CETP#
35
学习
58