海绵状血管瘤:术前设计切除范围很重要
2017-12-29 牛晓辉 郝林 骨肿瘤
海绵状血管瘤通常体积较大,自行消退的可能性很小,故通常需要手术治疗。为防止复发,如何设计切除范围?详见以下病例——
海绵状血管瘤通常体积较大,自行消退的可能性很小,故通常需要手术治疗。为防止复发,如何设计切除范围?详见以下病例——
(1)病例介绍
:患者,女,12岁,主因右大腿外侧疼痛5年,加重半年,于2003年6月入院。患者自5年前开始无明显诱因自觉右大腿近端外侧疼痛,当时不伴肿胀、包块,不影响活动,未诊治。半年前无明显诱因出现疼痛加重,活动后明显,休息可缓解,伴局部肿胀,可触及包块,至当地医院,B 超发现软组织肿物,即来我院就诊。

图23‐1 术前X 线片示右股骨上段正位,可见外侧软组织肿块影
入院查体:全身一般状况可,右大腿近端外侧肿胀,局部皮肤颜色正常,皮温稍高,可见浅表静脉曲张,可触及约15cm ×10cm 质软包块,位于筋膜深层,边界不清,活动度差,有压痛,患侧肢体活动因疼痛受限。
影像学检查:X 线表现(图23‐1):右大腿外侧可见软组织肿物影,质地不均匀,边界不清。B 超表现为右大腿外侧中上段肌层内可见一11.7cm×5.2cm×2.3cm低回声,不均匀,边界不清楚,内有血流信号,考虑海绵状血管瘤可能性大。MRI 表现(图23‐2):筋膜深层肌间隙内肿物,T 1呈不均匀高信号,T 2呈不均匀稍高信号,抑脂像呈高信号,增强明显不均匀强化。
入院后行穿刺活检,病理诊为局灶血管瘤样改变。于2003年7月行右大腿肿瘤局部切除术,术中见肿物位于阔筋膜深层,侵及阔筋膜张肌及部分臀中肌,将全部肿物连同阔筋膜、阔筋膜张肌及部分臀中肌一并切除(图23‐3),标本大体外观(图23‐4)为紫色质软组织,内有血窦,病理诊断为海绵状血管瘤。
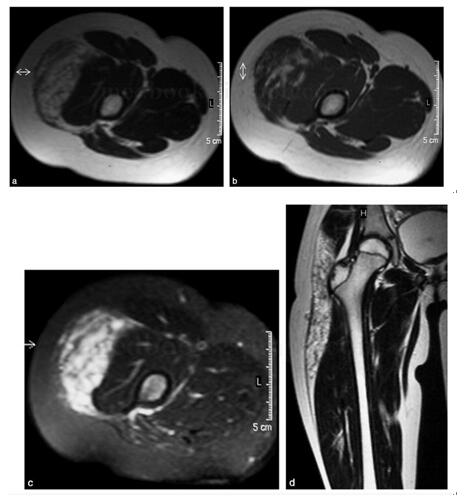
图23‐2 肿瘤M RI 表现 a﹒T 1 WI,示筋膜深层肌间隙内肿物,不均匀高信号;b﹒T 2 WI,示不均匀稍高信号;c﹒抑脂像呈高信号,增强明显不均匀强化;d﹒冠状位示肿瘤范围
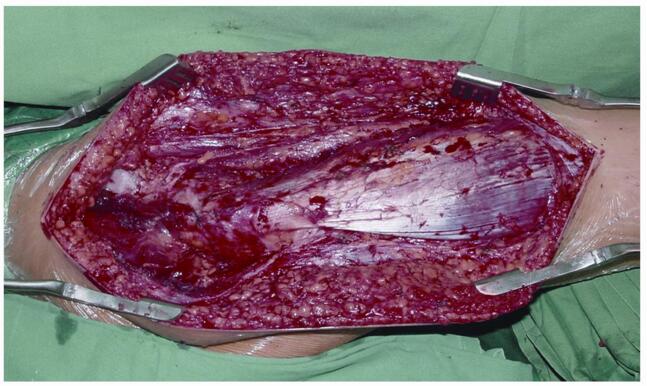
图23‐3 术中示肿瘤切除后范围
(2)专家分析
:海绵状血管瘤是由大量充满血液的腔隙或血窦所形成的血管瘤,腔壁上附有内皮细胞,腔隙间有纤维结缔组织间隔。先天性疾病,根据肿瘤生长快慢不同,可于各个年龄段出现症状,发生部位以四肢、躯干和面颈部为多,症状主要为疼痛,活动后可加重,休息可缓解。查体方面可表现为软组织肿块,边界不清,有压痛,很多患者包块常常不明显,但有明确的压痛点,而且多数病程较长。患者由于疼痛影响活动,可导致患肢肌肉萎缩,其周径反而小于健侧。影像学方面,X 线有时可见软组织肿块影,不具特异性;B 超有较典型表现,对于定性诊断有较高价值;对于体积较大病变,为明确病灶侵及范围、深度、累及周围组织程度及与主要血管关系等,MRI 可以发挥较大的作用。病理方面,大体切面呈海绵状或蜂窝状,含大量血液,镜下可见大量薄壁血管,管腔大且不规则,间质为纤维性,病程长者可发生钙化或骨化。
图23‐4 标本像示肿瘤血管呈紫色,向周围组织内浸润,与肌肉关系密切
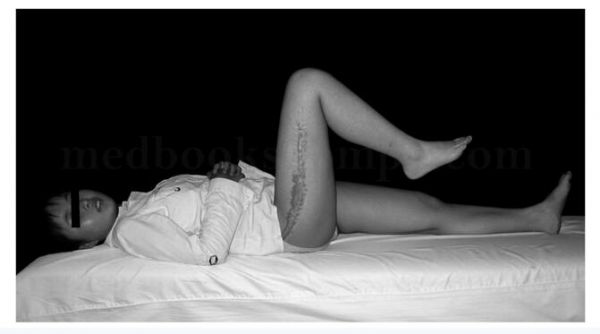
图23‐5 术后3年体位像示手术瘢痕范围,术后功能良好
良性血管瘤通常病程较长,如有典型临床表现,行相应B 超或MRI 检查,则可得到较明确的诊断。但若早期肿块不明显,仅有疼痛症状时,也易导致误诊。因此,详细询问病史和全面、认真的查体是非常必要的。通过穿刺活检可以得到病理学的诊断,可对鉴别肿瘤的良恶性有所帮助。由于其病程通常较长,就诊时通常肿瘤范围较广,可能累及主要肌肉,导致术后肢体功能损失较为严重。反之若残留异常血管,则复发率较高,难以达到治疗目的。故在明确诊断之后,应根据MRI 等影像学资料,仔细评估肿瘤范围及其与周围组织的关系,在保证肿瘤切除边界的前提下,尽可能保留功能或设法重建功能,术前应与患者及家属达成良好沟通,告知手术期望达到的效果及对术后功能造成的影响。由于此肿瘤内富含血液,且通常与周围主要血管关系紧密,故切勿低估术中失血,应做充分准备,术中注意达到术前设计的切除边界,并及时止血。术后应定期复查,警惕复发。

图23‐6 术后3年X 线片示右股骨上段正位,未见软组织肿块影
(3)诊断要点
:根据患者临床表现,主要为病程较长,局部疼痛伴或不伴包块,查体发现包块、固定压痛点及患肢肌萎缩,应警惕血管瘤可能,此时可行B 超检查以定性,行MRI 以明确病变范围及其与周围组织关系。应常规行穿刺活检以明确病理诊断。若病程较短,发展迅猛,则更需警惕恶性的可能。
(4)治疗原则
:海绵状血管瘤通常体积较大,自行消退的可能性很小,故通常需要手术治疗。术前应根据影像学仔细设计切除范围,应达到边缘或更佳的外科边界,以防止复发。术中应贯彻执行术前计划,警惕大出血。术后注意功能恢复情况,并叮嘱患者定期复查。
(5)随诊结果
:患者术后恢复良好,未见复发迹象。术后3年复查,局部功能良好(图23‐5),X 线未见软组织肿块(图23‐6)。
(6)经验教训
1)根据较典型的临床表现,行有针对性的影像学检查,明确诊断,避免误诊误治。行穿刺活检,病理诊断与临床及影像学相符。2)术前设计切除范围,达到良好外科边界,从而避免复发带给患者多次痛苦。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习一下谢谢分享
57
学习了谢谢分享
63
#血管瘤#
31
#海绵状血管瘤#
43
#海绵状#
24
学习
62