Adv mater:研究发现超声空化作用可增强声动力治疗效果
2018-06-05 佚名 声学研究所
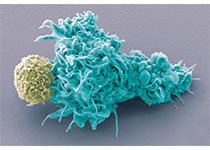
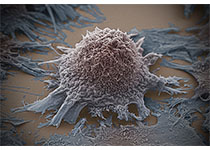
肿瘤是威胁人类健康的最危险疾病。作为一种新型肿瘤治疗技术,声动力疗法利用超声的强大穿透能力,深入组织内部,激活声敏剂产生活性氧进而杀伤肿瘤细胞,达到治疗目的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#治疗效果#
0
#研究发现#
24
谢谢梅斯提供这么好的信息,学到很多
46
不错的文章值得拥有哦
80
看看
47
学习谢谢分享
47
谢谢分享.学习了
46