病例(一)
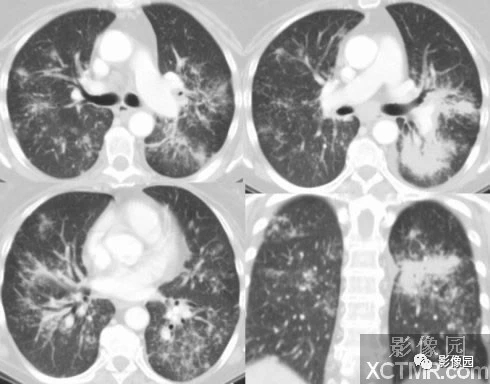
病史:男性,肺部反复发作的症状一直被当作肺炎治疗,呼吸衰竭。
CT表现:双肺明显大片状肺实变影,边界清楚或模糊,其内可见支气管显著扩张;周围仍可见正常的肺组织存在;右肺上叶呈肿块样完全实变。双侧胸腔少量积液。
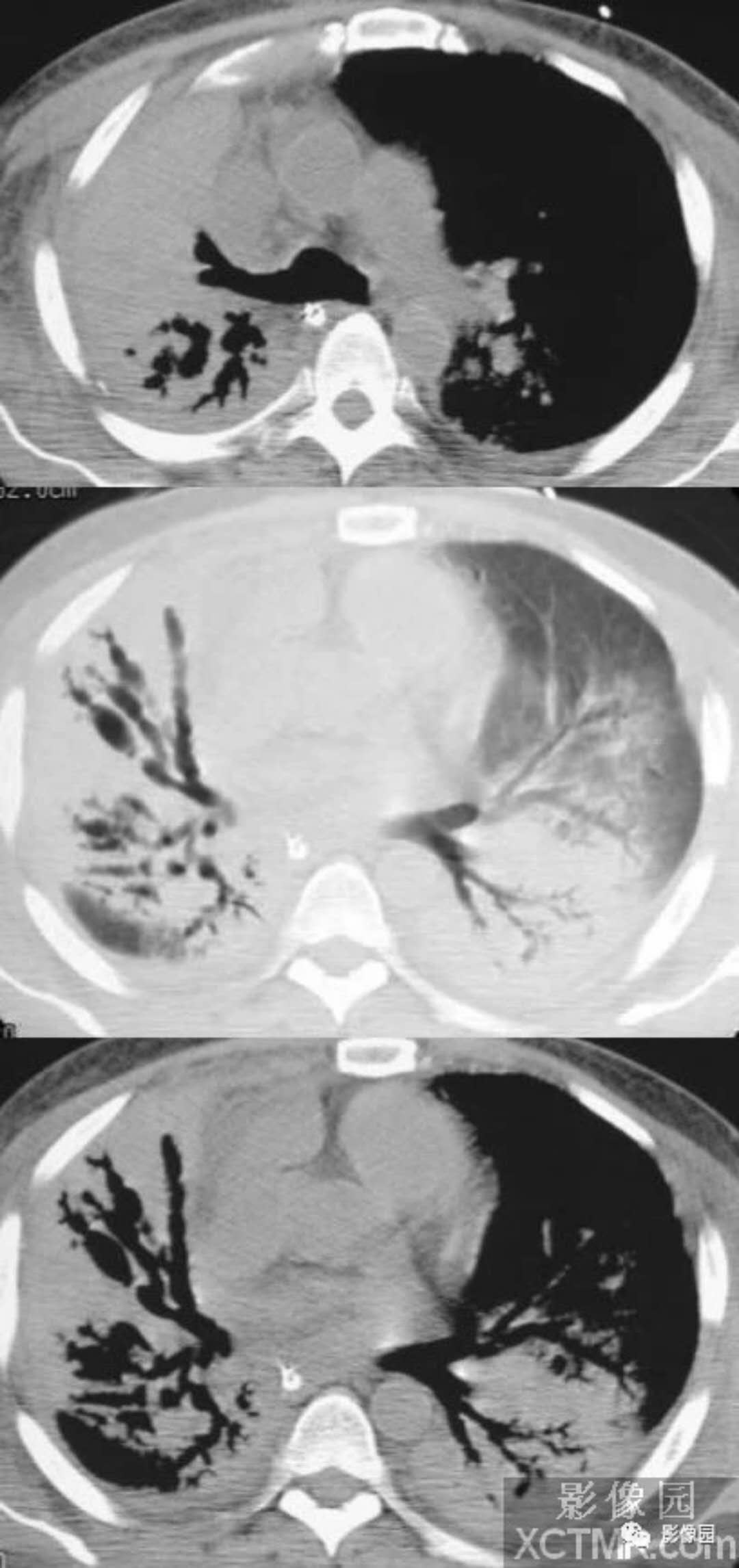
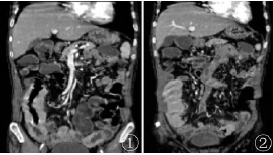
病例(二)
病史:女,气短数周。
X表现:双肺多发斑片状阴影,边界模糊,左肺比右肺明显。
CT表现:双肺斑片状实变影,散在多发小结节影,边界不清楚,部分有融合,主要沿支气管血管束分布。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#原发性#
45
#CT病例#
47
谢谢分享学习
77
谢谢分享学习
81
典型病例讨论.谢谢分享!
82