【一般资料】
患者,男,52岁,
【主诉】
因右后上牙龈肿物快速生长伴牙齿松动2个月于2014年06月22日来我院就诊,
【既往史】
既往有银屑病史,治疗情况不详。
【体格检查】
右侧鼻面沟膨隆,触之质硬;右侧鼻腔无通畅,无流血,右侧眶下区无感觉迟钝。双眼视物清,无复视。张口度及咬合关系正常,15~17处前庭沟隆起,乒乓球感不明显。颊侧牙龈可见一约3cm×3cm外生型肿物,边界清,表面呈桑葚状改变,覆盖15、16、17颊侧牙冠,质韧,触痛(-),探之不易出血,17、18松动II度,无叩痛,局部未扪及肿大淋巴结。
【辅助检查】
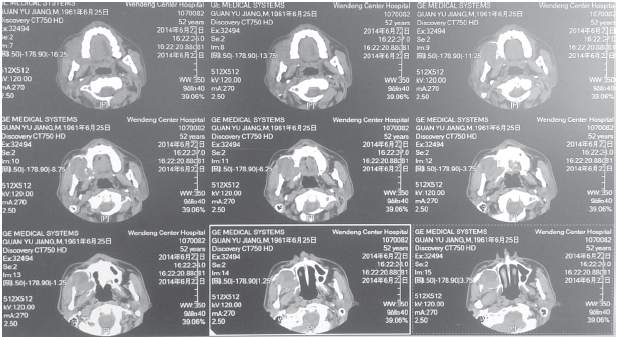
上颌骨CT(图1)示右侧上颌骨骨质呈颊舌向膨胀性破坏,边缘不完整,单房,病灶为囊实性改变,密度不均匀。未见明显骨性分离,未见切迹。右侧上颌窦壁受压变薄,下外侧壁不完整,上颌窦内见软组织影。向下突向上颌牙槽,延及牙龈。全颌曲面体层片见病灶侵犯牙槽突,14~18根尖位于病灶内,且呈截根样改变。其他辅助检查结果未见明显手术禁忌。
【初步诊断】
右上颌骨肿物,成釉细胞瘤?
【治疗】
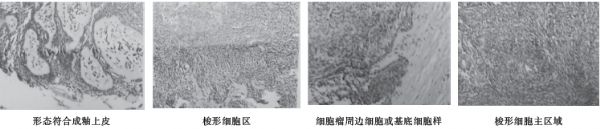
全麻生效后完整切取牙龈病变及临界组织行冰冻检查,示:病变复合成釉细胞瘤,肿瘤内见核分裂及坏死。于上唇唇红正中向上沿人中沟、右侧鼻底、右侧鼻面沟、右侧内眦、眶下缘至右侧外眦切开软组织,同时切开右侧上颌前庭沟,向外翻开软组织瓣,暴露上颌骨,见:上颌骨内囊实性肿物,约4cm×3cm,呈暗红色,与周围软组织粘连明显。肿物累及上颌窦,上颌窦下前壁部分骨质吸收,上壁及内侧壁较完整,尚未累积眼球及鼻腔。右上颌牙槽突吸收,14~18根尖呈截根状改变。保留右侧眶下壁及右侧鼻外侧壁,分离右上颌腭侧黏骨膜瓣,将肿物及部分上颌骨切除(包括右上4、5、6、7、8牙齿)。冲洗创腔,无活动性出血后,放置碘仿砂团,分层缝合切口。术后给予抗炎、止血、补液等对症治疗。术后10~17d分次取出碘仿砂条。病愈出院。术后病理:右上颌成釉细胞瘤,生长活跃,以梭形细胞型及丛状型生长方式为主。肉眼见肿物剖面灰黄,质韧,伴有囊变。镜检(图2):上颌肿物,形态复合成釉上皮,以梭形细胞为主,丛状生长方式,周边呈基底细胞样排列。
原始出处:
孙晓宇, 王静. 上颌骨成釉细胞瘤病例1例报道[J]. 临床合理用药杂志, 2017, 10(2):163-164.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#上颌骨#
20
#成釉细胞#
30
#细胞瘤#
27
#上颌#
21
谢谢分享.学习了
50