Stroke:AHA/ASA发布卒中后脑水肿管理指南
2014-02-18 安荷娣 根据《急性脑血管病所致双眼睑下垂三例》
美国心脏协会/美国卒中协会(AHA/ASA)发布了《大脑和小脑梗死伴脑水肿的管理推荐科学声明》,该指南旨在为卒中相关医师、神经外科医师、康复医师和急诊医师进行临床决策提供依据,为患者提供最好的综合治疗方案。该指南经过了广泛的AHA内部同行评议,指南全文2014年1月30日在线发表于《卒中》Stroke杂志。 指南制定者指出,大脑和小脑水肿是需要给予快速、专业神经重症监护并常常需要给予神经外科干预
美国心脏协会/美国卒中协会(AHA/ASA)发布了《大脑和小脑梗死伴脑水肿的管理推荐科学声明》,该指南旨在为卒中相关医师、神经外科医师、康复医师和急诊医师进行临床决策提供依据,为患者提供最好的综合治疗方案。该指南经过了广泛的AHA内部同行评议,指南全文2014年1月30日在线发表于《卒中》Stroke杂志。【原文下载】
指南制定者指出,大脑和小脑水肿是需要给予快速、专业神经重症监护并常常需要给予神经外科干预的临界条件。许多患者需要进行去骨瓣减压术治疗,选择这种治疗的患者将有极大的获益,虽然会留下一些后遗症,但他们可能会实现功能独立。
主要作者、梅奥诊所的神经重症专家Eelco F.M. Wijdicks博士认为,我们的经验是卒中伴脑水肿患者积极采用上述治疗可能获得良好的结局。
Wijdicks博士说,多年来基于药物和手术治疗的良好证据,我们形成了复杂的卒中管理方案。指南汇总了相关的证据,将有助于帮助该组患者做出正确的临床决策。
Wijdicks博士指出,这是首次将半球(涉及整个大脑中动脉供血区或更大范围)和小脑(涉及小脑后下动脉或小脑上动脉)两种卒中类型的水肿放到一个文件中讨论,指南全面陈述了多种综合管理选项。
哪些患者需要手术?
Wijdicks博士解释,脑水肿通常出现在大面积脑卒中的患者,患者常因此死亡。“我们想了解一下这些患者的选择。”早期去骨瓣减压术可以帮助许多患者,但是手术需要移除一般的颅骨,有许多潜在的并发症。关键问题是,我们应该如何判断哪些患者需要进行手术?这一问题没有明确答案,但我们列出了几项需要考虑的原则。
一般来说,年轻患者进行手术获益最大。例如,一个30岁的患者发生大面积脑卒中伴脑水肿应该立即进行手术;而超过60岁的患者则不建议进行手术。
其他需要考虑的因素包括患者积极实施康复治疗计划的能力和发病前的健康状态。许多后勤方面的因素也需要加以考虑,患者必须转运到能够实施该手术的医院,可能距离很远。年轻的大面积脑卒中患者即使没有脑水肿也应该转院,因为随病情进展可能出现脑水肿。
指南指出,幕上半球缺血性卒中可能恶化的临床表现包括出现意识障碍或意识障碍加重、脑性上睑下垂、瞳孔大小变化。小脑梗死水肿时若脑干受压会出现意识水平下降。因此,可能出现早期角膜反射迟钝和瞳孔缩小。
如何进行综合管理?
作者建议,应建立标准化的定义以促进多中心、基于人群的发病率、患病率、危险因素和预后研究。识别脑水肿高危患者应包括临床和神经影像数据。
指南指出,大面积脑卒中患者的全面康复需要具备神经功能监测能力的单元(卒中单元)。患者最好收住重症监护病房或卒中单元,由技能熟练、经验丰富的医师主管,如神经重症专家或血管神经病学专家。
综合医疗护理包括气道管理和机械通气、血压管理、液体管理、血糖管理和体温管理等。
幕上半球缺血性卒中伴脑水肿,应常规进行颅内压监测,不需进行脑脊液引流;但神经功能继续恶化的患者应考虑给予去骨瓣减压术及硬脑膜扩张。≥60岁的患者进行去骨瓣减压术的疗效不确定。
小脑卒中脑水肿且神经功能恶化的患者应进行枕骨下颅骨切除术及硬脑膜扩张。在枕骨下颅骨切除术的同时应进行脑室造瘘术以缓解梗阻性脑积水,以防小脑位置上移引起病情恶化。
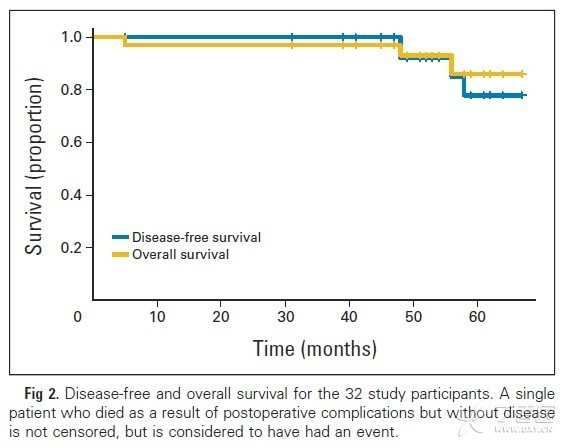
幕上半球脑梗死伴脑水肿可以获得令人满意的预后,但应预见到1/3的患者会出现重度残疾和完全依赖,即使给予去骨瓣减压术。指南指出,大多数患者小脑梗死患者手术后可以获得一个可接受的功能预后。
原始出处
Wijdicks EF, Sheth KN, Carter BS, Greer DM, Kasner SE, Kimberly WT, Schwab S, Smith EE, Tamargo RJ, Wintermark M; on behalf of the American Heart Association Stroke Council.Recommendations for the Management of Cerebral and Cerebellar Infarction With Swelling: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association.Stroke. 2014 Jan 30.【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASA#
38
#卒中后#
40
#管理指南#
35
主要还是神经外科的办法,药物脱水没提及太多
110
#脑水肿#
34
#AHA#
25
#水肿#
30