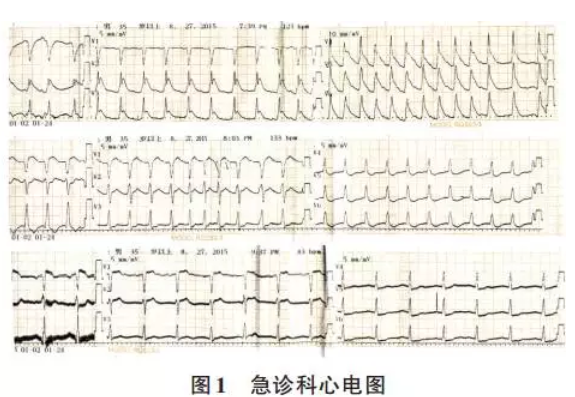
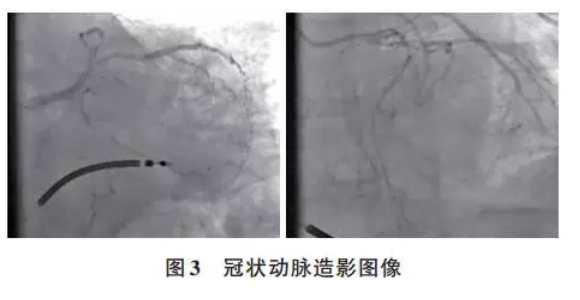
病例分享:急性冠状动脉综合征致短QT间期致心室电风暴1例
2017-10-21 高燕男等 岭南心血管杂志
患者,男,47岁,突发心跳骤停,心肺复苏术后15 min入急诊科。不久后发生心室电风暴。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#电风暴#
39
#冠状动脉综合征#
33
#QT间期#
32
#综合征#
37
非常棒的内容呢.认真学习
49
很好很好很好
44